Neueste Videos

EART (Health Education and Rescue Training) Wilderness First Aid is an intensive course that covers patient examination and evaluation, body systems and anatomy, wound care, splinting, environmental emergencies, and backcountry medicine. Hands-on simulations provide first-hand training in treating patients. This is an excellent course taught by experienced Wilderness First Responders and Emergency Medical Technicians and is highly recommended to all wilderness travelers. People who pass the courses will receive a Wilderness First Aid certification from the Emergency Care and Safety Institute (ECSI) which is good for 2 years. Participants who successfully pass CPR and HEART Wilderness First Aid will have met the First Aid requirements for OA Leader Training.
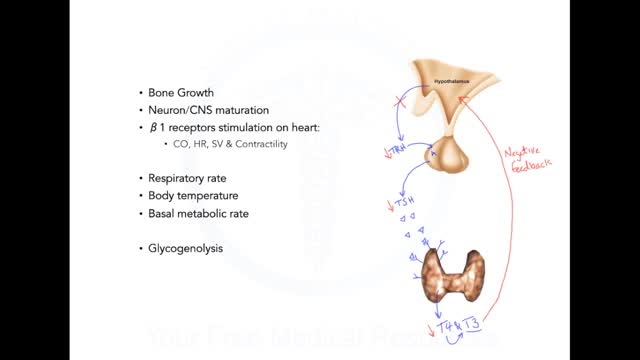
Graves disease is an autoimmune disorder that leads to an overactive thyroid gland (hyperthyroidism). An autoimmune disorder is a condition that occurs when the immune system mistakenly attacks healthy tissue. Causes The thyroid gland is an important organ of the endocrine system. The gland is located at the front of the neck above where the collarbones meet. This gland releases the hormones thyroxine (T4) and triiodothyronine (T3), which control body metabolism. Controlling metabolism is important for regulating mood, weight, and mental and physical energy levels. When the body makes too much thyroid hormone, the condition is called hyperthyroidism. (An underactive thyroid leads to hypothyroidism.) Graves disease is the most common cause of hyperthyroidism. It is due to an abnormal immune system response that causes the thyroid gland to produce too much thyroid hormone. Graves disease is most common in women over age 20. But the disorder can occur at any age and can affect men as well. Symptoms Younger people may have these symptoms: Anxiety or nervousness, as well as problems sleeping Breast enlargement in men (possible) Problems concentrating Fatigue Frequent bowel movements Hair loss Heat intolerance and increased sweating Increased appetite, despite having weight loss Irregular menstrual periods in women Muscle weakness of the hips and shoulders Moodiness, including irritability and anger Rapid or irregular heartbeat Shortness of breath with activity Tremor Many people with Graves disease have problems with their eyes: The eyeballs may seem to be bulging out and may be painful. Eyes can feel irritated and be tearing. Double vision may be present. Older people may have these symptoms: Rapid or irregular heartbeat Chest pain Memory loss Weakness and fatigue

You might not notice signs or symptoms of Hashimoto's disease at first, or you may notice a swelling at the front of your throat (goiter). Hashimoto's disease typically progresses slowly over years and causes chronic thyroid damage, leading to a drop in thyroid hormone levels in your blood. The signs and symptoms are mainly those of an underactive thyroid gland (hypothyroidism). Signs and symptoms of hypothyroidism include: Fatigue and sluggishness Increased sensitivity to cold Constipation Pale, dry skin A puffy face Hoarse voice Unexplained weight gain — occurring infrequently and rarely exceeding 10 to 20 pounds, most of which is fluid Muscle aches, tenderness and stiffness, especially in your shoulders and hips Pain and stiffness in your joints and swelling in your knees or the small joints in your hands and feet Muscle weakness, especially in your lower extremities Excessive or prolonged menstrual bleeding (menorrhagia) Depression

Heat stroke is the most serious form of heat injury and is considered a medical emergency. If you suspect that someone has heat stroke -- also known as sunstroke -- call 911 immediately and give first aid until paramedics arrive. Heat stroke can kill or cause damage to the brain and other internal organs. Although heat stroke mainly affects people over age 50, it also takes a toll on healthy young athletes. Heat stroke often occurs as a progression from milder heat-related illnesses such as heat cramps, heat syncope (fainting), and heat exhaustion. But it can strike even if you have no previous signs of heat injury. Heat stroke results from prolonged exposure to high temperatures -- usually in combination with dehydration -- which leads to failure of the body's temperature control system. The medical definition of heat stroke is a core body temperature greater than 105 degrees Fahrenheit, with complications involving the central nervous system that occur after exposure to high temperatures. Other common symptoms include nausea, seizures, confusion, disorientation, and sometimes loss of consciousness or coma
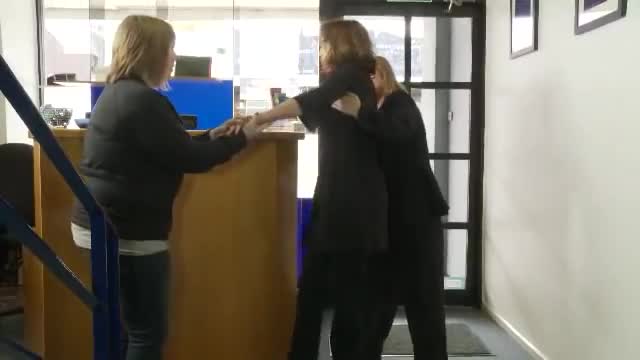
Fainting occurs when the blood supply to your brain is momentarily inadequate, causing you to lose consciousness. This loss of consciousness is usually brief. Fainting can have no medical significance, or the cause can be a serious disorder. Therefore, treat loss of consciousness as a medical emergency until the signs and symptoms are relieved and the cause is known. Discuss recurrent fainting spells with your doctor. If you feel faint Lie down or sit down. To reduce the chance of fainting again, don't get up too quickly. Place your head between your knees if you sit down. If someone else faints Position the person on his or her back. If the person is breathing, restore blood flow to the brain by raising the person's legs above heart level — about 12 inches (30 centimeters) — if possible. Loosen belts, collars or other constrictive clothing. To reduce the chance of fainting again, don't get the person up too quickly. If the person doesn't regain consciousness within one minute, call 911 or your local emergency number. Check the person's airway to be sure it's clear. Watch for vomiting. Check for signs of circulation (breathing, coughing or movement). If absent, begin CPR. Call 911 or your local emergency number. Continue CPR until help arrives or the person responds and begins to breathe.

Approximately 10%-15% of human bite wounds become infected owing to multiple factors. The bacterial inoculum of human bite wounds contains as many as 100 million organisms per milliliter and is made up of as many as 190 different species. Many of these are anaerobes that flourish in the low redox environment of tartar that lies between human teeth or in areas of gingivitis. Most injuries due to human bites involve the hands. Hand wounds, regardless of the etiology, have a higher rate of infection than do those in other a locations. (See Pathophysiology and Etiology.) Infections associated with human bites are often far advanced by the time they receive appropriate care. Patients often wait until infection is well established before seeking medical treatment. These wounds are frequently more extensive than estimated on initial examination by the inexperienced observer and are frequently managed inadequately. (See Prognosis, Presentation, Treatment, and Medication.) Human bites have been shown to transmit hepatitis B, hepatitis C, herpes simplex virus (HSV), syphilis, tuberculosis, actinomycosis, and tetanus. Evidence suggests that it is biologically possible, but quite unlikely, to transmit human immunodeficiency virus (HIV) through human bites. (See Pathophysiology, Presentation, and Workup.)
Breast Cancer Screening Recommendations Breast cancer screening is important for all women. If you are at higher risk of breast cancer, you may need to be screened earlier and more often than women at average risk. Breast cancer screening is only recommended for some men at very high risk due to an inherited gene mutation or a strong family history of breast cancer.
Colorectal cancer screening tests Screening is the process of looking for cancer in people who have no symptoms of the disease. Several tests can be used to screen for colorectal cancers. These tests can be divided into: Tests that can find both colorectal polyps and cancer: These tests look at the structure of the colon itself to find any abnormal areas. This is done either with a scope put into the rectum or with special imaging (x-ray) tests. Polyps found during these tests can be removed before they become cancerous, so these tests may prevent colorectal cancer. Because of this, these tests are preferred if they are available and you are willing to have them. Tests that mainly find cancer: These tests check the stool (feces) for signs of cancer. These tests are less invasive and easier to have done, but they are less likely to detect polyps.
Skin changes are among the most visible signs of aging. Evidence of increasing age includes wrinkles and sagging skin. Whitening or graying of the hair is another obvious sign of aging. Your skin does many things. It: Contains nerve receptors that allow you to feel touch, pain, and pressure Helps control fluid and electrolyte balance Helps control your body temperature Protects you from the environment Although skin has many layers, it can generally be divided into three main parts: The outer part (epidermis) contains skin cells, pigment, and proteins. The middle part (dermis) contains blood vessels, nerves, hair follicles, and oil glands. The dermis provides nutrients to the epidermis. The inner layer under the dermis (the subcutaneous layer) contains sweat glands, some hair follicles, blood vessels, and fat. Each layer also contains connective tissue with collagen fibers to give support and elastin fibers to provide flexibility and strength.
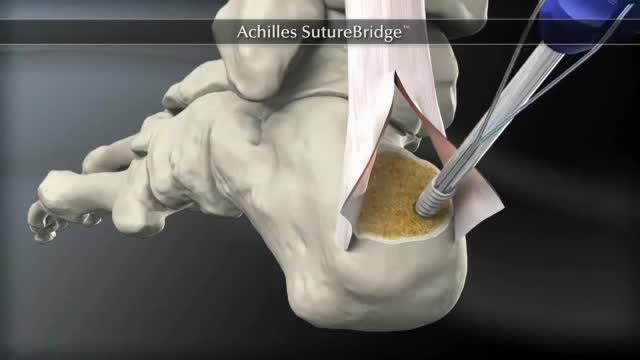
The Arthrex SpeedBridge™ is an innovative soft tissue fixation device used in the treatment of Achilles injuries. While standard anchor fixation of the tendon creates only a single point of compression directly over the anchor, the SpeedBridge enables an hourglass pattern of FiberTape® suture to be laid over the distal end of the tendon. This four-anchor construct enables a true knotless repair and a greater area of compression for the Achilles tendon on the calcaneus, improving stability and possibly allowing for earlier return to normal activities.

Breast cancer usually starts off in the inner lining of milk ducts or the lobules that supply them with milk. A malignant tumor can spread to other parts of the body. A breast cancer that started off in the lobules is known as lobular carcinoma, while one that developed from the ducts is called ductal carcinoma. The vast majority of breast cancer cases occur in females. This article focuses on breast cancer in women. We also have an article about male breast cancer. Breast cancer is the most common invasive cancer in females worldwide. It accounts for 16% of all female cancers and 22.9% of invasive cancers in women. 18.2% of all cancer deaths worldwide, including both males and females, are from breast cancer. Breast cancer rates are much higher in developed nations compared to developing ones. There are several reasons for this, with possibly life-expectancy being one of the key factors - breast cancer is more common in elderly women; women in the richest countries live much longer than those in the poorest nations. The different lifestyles and eating habits of females in rich and poor countries are also contributory factors, experts believe. According to the National Cancer Institute, 232,340 female breast cancers and 2,240 male breast cancers are reported in the USA each year, as well as about 39,620 deaths caused by the disease.

The Zika virus, first identified in Uganda in 1947, is transmitted by the same type of mosquito that carries dengue fever, yellow fever, and chikungunya virus. A mosquito bites an infected person and then passes those viruses to other people it bites. Outbreaks did not occur outside of Africa until 2007, when it spread to the South Pacific.