Vascular Disease
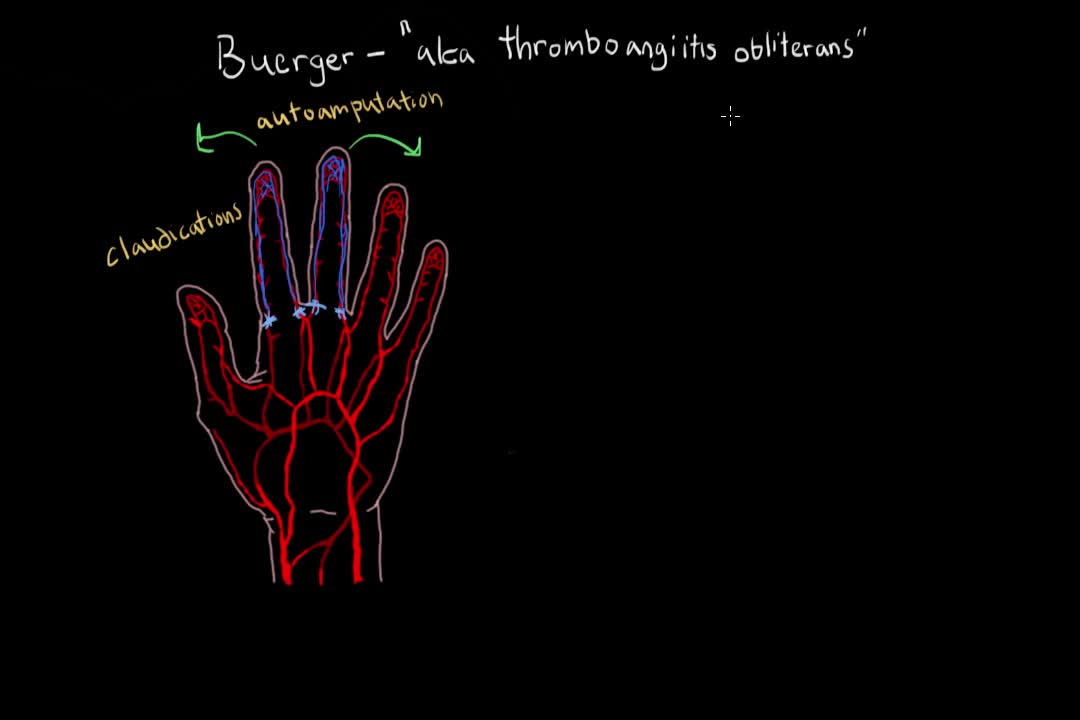
Buerger's disease (thromboangiitis obliterans) is a rare disease of the arteries and veins in the arms and legs. In Buerger's disease, your blood vessels become inflamed, swell and can become blocked with blood clots (thrombi). This eventually damages or destroys skin tissues and may lead to infection and gangrene. Buerger's disease usually first shows in your hands and feet and may eventually affect larger areas of your arms and legs. Virtually everyone diagnosed with Buerger's disease smokes cigarettes or uses other forms of tobacco, such as chewing tobacco. Quitting all forms of tobacco is the only way to stop Buerger's disease. For those who don't quit, amputation of all or part of a limb is sometimes necessary.
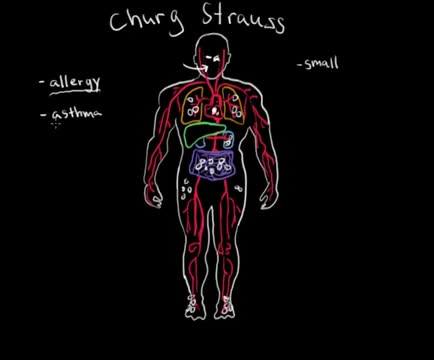
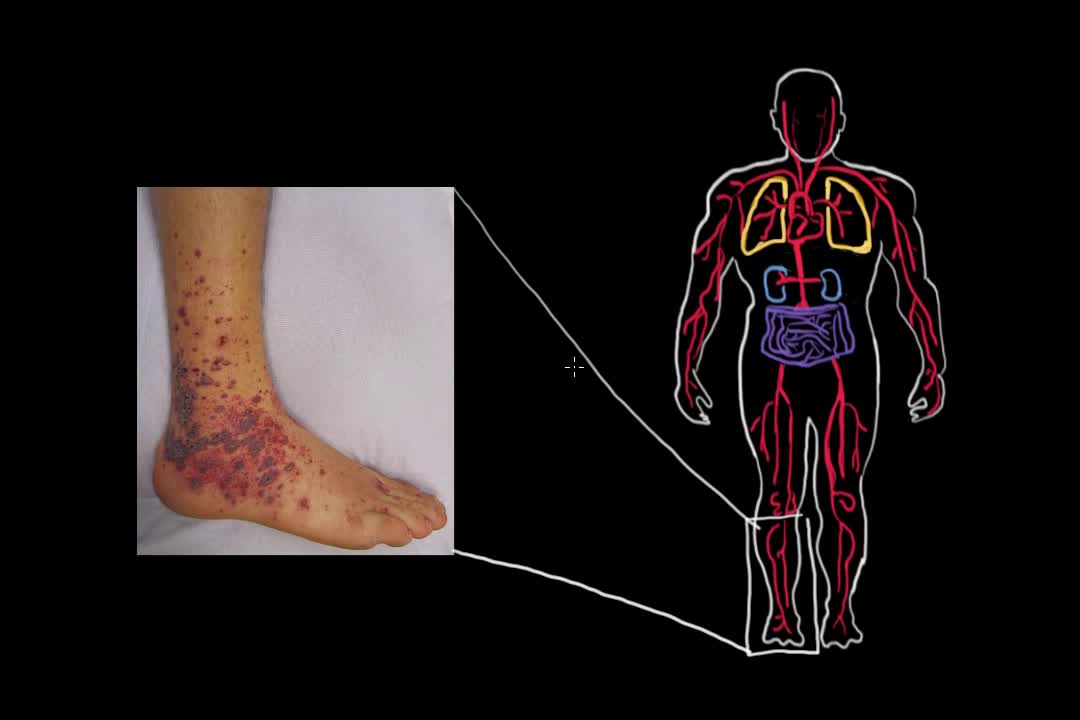
Eosinophilic granulomatosis with polyangiitis (EGPA)—or, as it was traditionally termed, Churg-Strauss syndrome—is a rare systemic necrotizing vasculitis that affects small-to-medium-sized vessels and is associated with severe asthma and blood and tissue eosinophilia. [1] Like granulomatosis with polyangiitis (Wegener granulomatosis), and the microscopic form of periarteritis (ie, microscopic polyangiitis), EGPA is an antineutrophil cytoplasmic antibody (ANCA)–associated vasculitide. [2, 3, 4, 5] In 1951, Churg and Strauss first described the syndrome in 13 patients who had asthma, eosinophilia, granulomatous inflammation, necrotizing systemic vasculitis, and necrotizing glomerulonephritis. [3] In 1990, the American College of Rheumatology (ACR) proposed the following six criteria for the diagnosis of Churg-Strauss syndrome [6] : Asthma (wheezing, expiratory rhonchi) Eosinophilia of more than 10% in peripheral blood Paranasal sinusitis Pulmonary infiltrates (may be transient) Histological proof of vasculitis with extravascular eosinophils Mononeuritis multiplex or polyneuropathy
Temporal arteritis is a condition in which the temporal arteries, which supply blood to the head and brain, become inflamed or damaged. It is also known as cranial arteritis or giant cell arteritis. Although this condition usually occurs in the temporal arteries, it can occur in almost any medium to large artery in the body. The journal Arthritis & Rheumatology states that approximately 228,000 people in the United States are affected by temporal arteritis. According to the American College of Rheumatology, people over the age of 50 are more likely than younger people to develop the condition. Women are also more likely than men to have temporal arteritis. It is most prevalent in people of northern European or Scandinavian descent. Although the exact cause of the condition is unknown, it may be linked to the body’s autoimmune response. Also, excessive doses of antibiotics and certain severe infections have been linked to temporal arteritis. There’s no known prevention. However, once diagnosed, temporal arteritis can be treated to minimize complications.
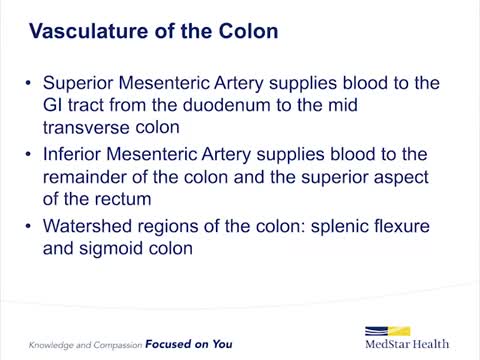
Ischemic colitis occurs when blood flow to part of the large intestine (colon) is reduced, usually due to narrowed or blocked blood vessels (arteries). The diminished blood flow doesn't provide enough oxygen for the cells in your digestive system. Ischemic colitis can cause pain and may damage your colon. Any part of the colon can be affected, but ischemic colitis usually causes pain on the left side of the belly area (abdomen). The condition can be misdiagnosed because it can easily be confused with other digestive problems. Ischemic colitis may heal on its own. But you may need medication to treat ischemic colitis or prevent infection, or you may need surgery if your colon has been damaged. Symptoms ShareTweet Oct. 13, 2015 References Products and Services Newsletter: Mayo Clinic Health Letter See also Abdominal pain Colonoscopy Color Blue Detects Colon Cancer CT scan CT scans: Are they safe? Diarrhea Ultrasound Advertisement Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Advertising & Sponsorship PolicyOpportunitiesAd Choices Mayo Clinic Store Check out these best-sellers and special offers on books and newsletters from Mayo Clinic. NEW! – The Mayo Clinic Diet, Second Edition Treatment Strategies for Arthritis Mayo Clinic on Better Hearing and Balance Keeping your bones healthy and strong The Mayo Clinic Diet Online Ads by Swoop Psoriasis Treatment www.informationaboutpsoriasis.com Explore a Treatment Option for Moderate to Severe Plaque Psoriasis Immune Biomarker PD-L1 - Discover the Science iobiomarkers.bmsinformation.com Understanding Assay Results for PD-L1 is Crucial for Treatment Decisions. Biomarker PD-L1 Information - Easy to Download Resources iobiomarkers.bmsinformation.com Explore the Role of PD-L1 in Immuno-Oncology & the Evolving Biomarker Landscape.

Chronic mesenteric ischemia (CMI) usually results from long-standing atherosclerotic disease of 2 or more mesenteric vessels. [1] Other nonatheromatous causes of CMI include the vasculitides, such as Takayasu arteritis. Symptoms are caused by the gradual reduction in blood flow to the intestine. [2] (See Presentation.) In 1958, Shaw and Maynard described the first thromboendarterectomy of the superior mesenteric artery (SMA) for the treatment of both acute mesenteric ischemia (AMI) and CMI. Several other surgical procedures have since been attempted, ranging from reimplantation of the visceral branch into the adjacent aorta to using an autogenous vein graft. In 1972, Stoney and Wylie introduced transaortic visceral thromboendarterectomy and aortovisceral bypass, which have proved to be highly effective techniques.
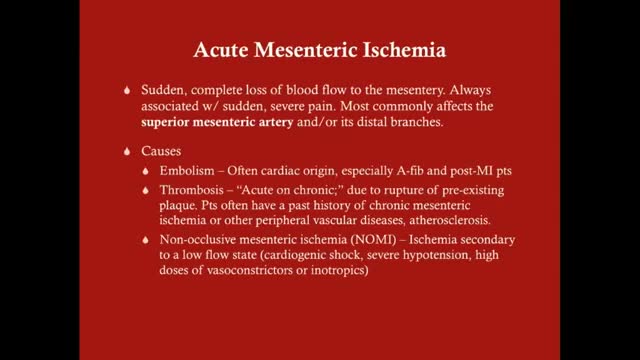
Acute mesenteric ischemia (AMI) is a syndrome caused by inadequate blood flow through the mesenteric vessels, resulting in ischemia and eventual gangrene of the bowel wall. Although relatively rare, it is a potentially life-threatening condition. Broadly, AMI may be classified as either arterial or venous. AMI as arterial disease may be subdivided into nonocclusive mesenteric ischemia (NOMI) and occlusive mesenteric arterial ischemia (OMAI); OMAI may be further subdivided into acute mesenteric arterial embolism (AMAE) and acute mesenteric arterial thrombosis (AMAT). AMI as venous disease takes the form of mesenteric venous thrombosis (MVT).
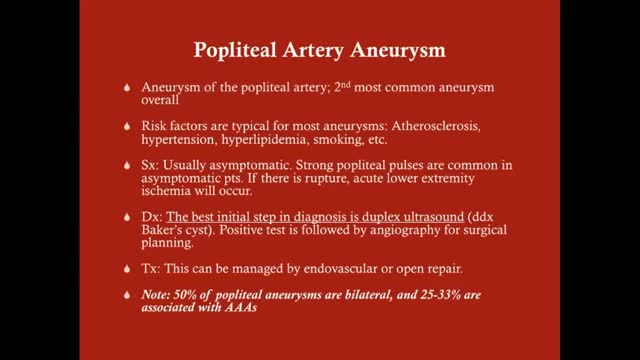
What is a brain aneurysm? A brain (cerebral) aneurysm is a bulging, weak area in the wall of an artery that supplies blood to the brain. In most cases, a brain aneurysm causes no symptoms and goes unnoticed. In rare cases, the brain aneurysm ruptures, releasing blood into the skull and causing a stroke. When a brain aneurysm ruptures, the result is called a subarachnoid hemorrhage. Depending on the severity of the hemorrhage, brain damage or death may result.
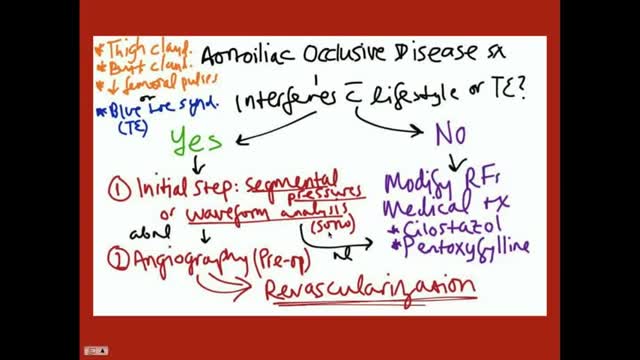
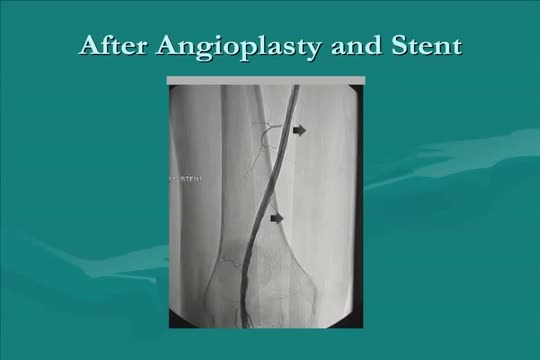
Aortoiliac occlusive disease (AIOD) occurs commonly in patients with PAD. Significant lesions in the aortoiliac arterial segment are exposed easily by palpation of the femoral pulses. Any diminution of the palpable femoral pulse indicates that a more proximal obstruction exists. Obstructive lesions may be present in the infrarenal aorta, common iliac, internal iliac (hypogastric), external iliac, or combinations of any or all of these vessels. Occasionally, degenerated nonstenotic atheromatous disease exists in these vessels and may manifest by atheroembolism to the foot, the "blue toe" or "trash foot" syndrome. Generally, patients with aortoiliac PAD have a poorer general prognosis than those with more distal PAD.
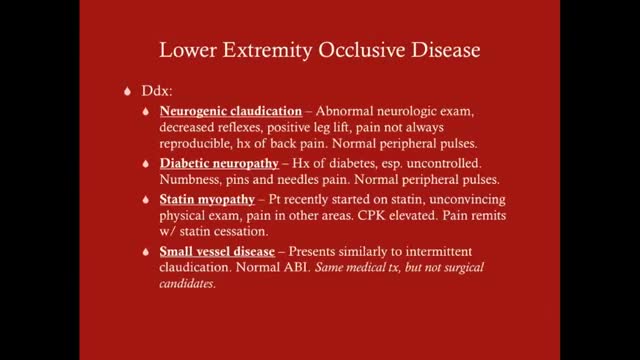
Claudication, which is defined as reproducible ischemic muscle pain, is one of the most common manifestations of peripheral arterial occlusive disease (PAOD) caused by atherosclerosis. Claudication occurs during physical activity and is relieved after a short rest. Pain develops because of inadequate blood flow. Examination of a patient with claudication should include a complete lower-extremity evaluation and pulse examination, including measuring segmental pressures. Attempt to palpate pulses from the abdominal aorta to the foot, with auscultation for bruits in the abdominal and pelvic regions. When palpable pulses are not present, a handheld Doppler device may be used to assess circulation.