সর্বশেষ ভিডিও

the motor milestones expected in typically developing babies, from head control to walking and what pediatricians look for during a well-baby visit. She also explains the specific types of motor control a baby must master before the next milestone can be achieved
The Distal Femoral Osteotomy System utilizes the same principles of design featured in the Tibial Osteotomy System. Specifically designed femoral osteotomy plates take into account the anatomical differences between the distal femur and proximal tibia.

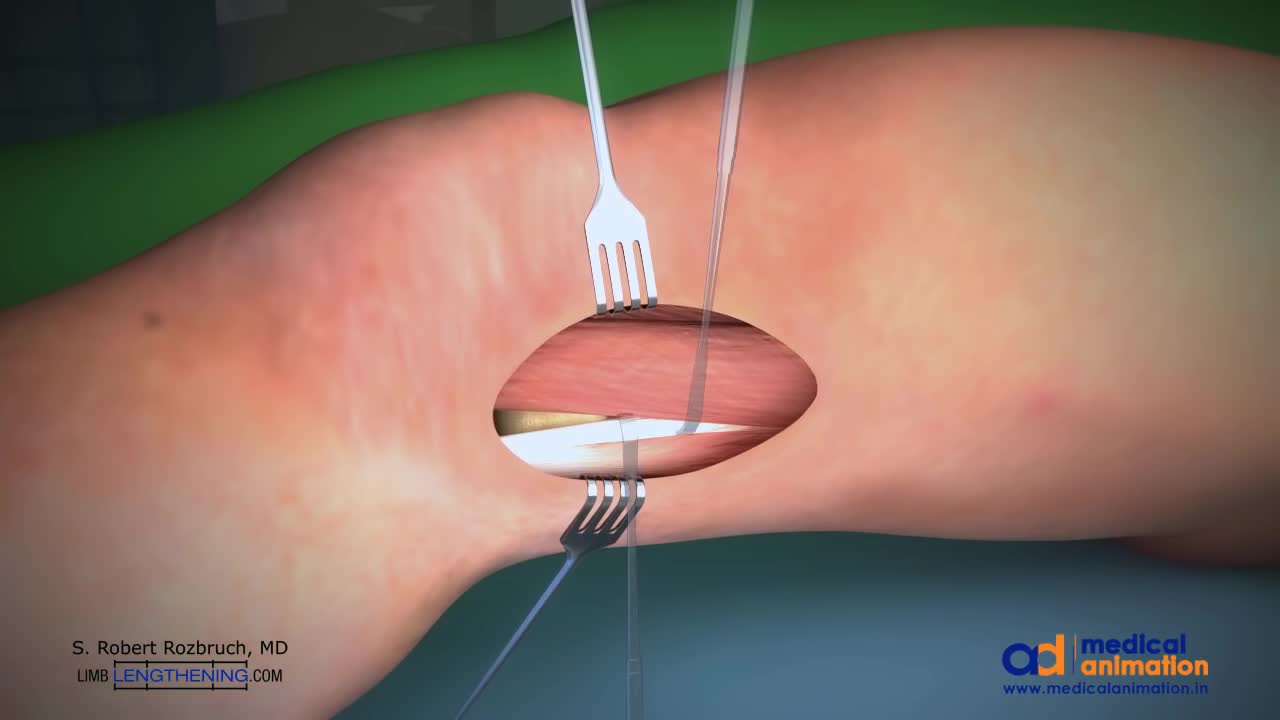
This is a technique of correcting knock knee (genu valgum) deformity by surgery. Highligh of the technique is that the bone is not cut, but merely weakened. The advantage is that it provides accuracy to the surgeon, and rapid healing. Once corrected, the bone is held in place with a special plate (Tomofix), which permits walking with crutches the very next day.
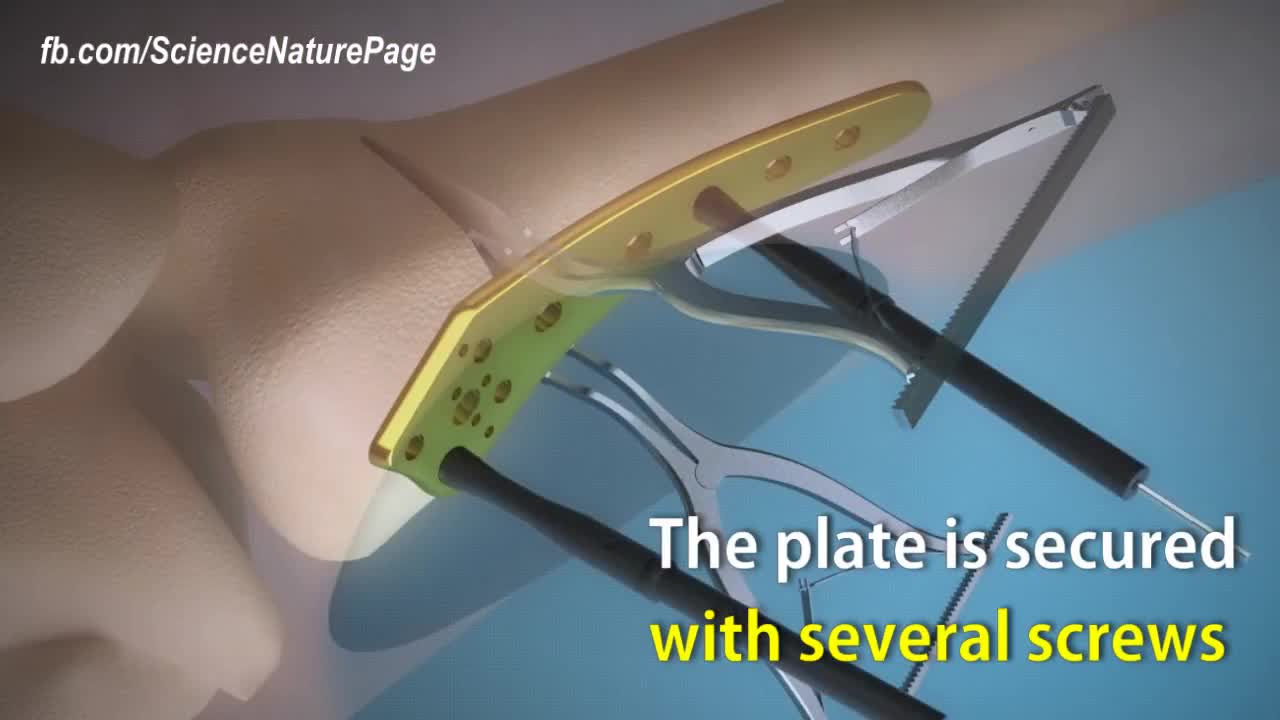
Here is how surgeons perform knock knee correction surgery. Titanium plate is used to stabilize the affected area. The femur is cut nearly through to help with the stability. Spreaders angle the cut align the leg. The plate is secured with several screws. Synthetic bone graft material is packed in the joint. The patient will be in crutches for 4 to 6 weeks.

When United Airlines decides their employees flying to Kentucky is more important than a doctor or any passenger who paid for their ticket it is time to STOP FLYING UNITED!!! Here are United employees dragging the man off the plane like a criminal.
A bone marrow biopsy removes a small amount of bone and a small amount of fluid and cells from inside the bone (bone marrow). A bone marrow aspiration removes only the marrow. These tests are often done to find the reason for many blood disorders and may be used to find out if cancer or infection has spread to the bone marrow. Bone marrow aspiration removes a small amount of bone marrow fluid and cells through a needle put into a bone. The bone marrow fluid and cells are checked for problems with any of the blood cells made in the bone marrow. Cells can be checked for chromosome problems. Cultures can also be done to look for infection. A bone marrow biopsy removes bone with the marrow inside to look at under a microscope. The aspiration (taking fluid) is usually done first, and then the biopsy.
Nuclear medicine is a branch of medical imaging that uses small amounts of radioactive material to diagnose and determine the severity of or treat a variety of diseases, including many types of cancers, heart disease, gastrointestinal, endocrine, neurological disorders and other abnormalities within the body.
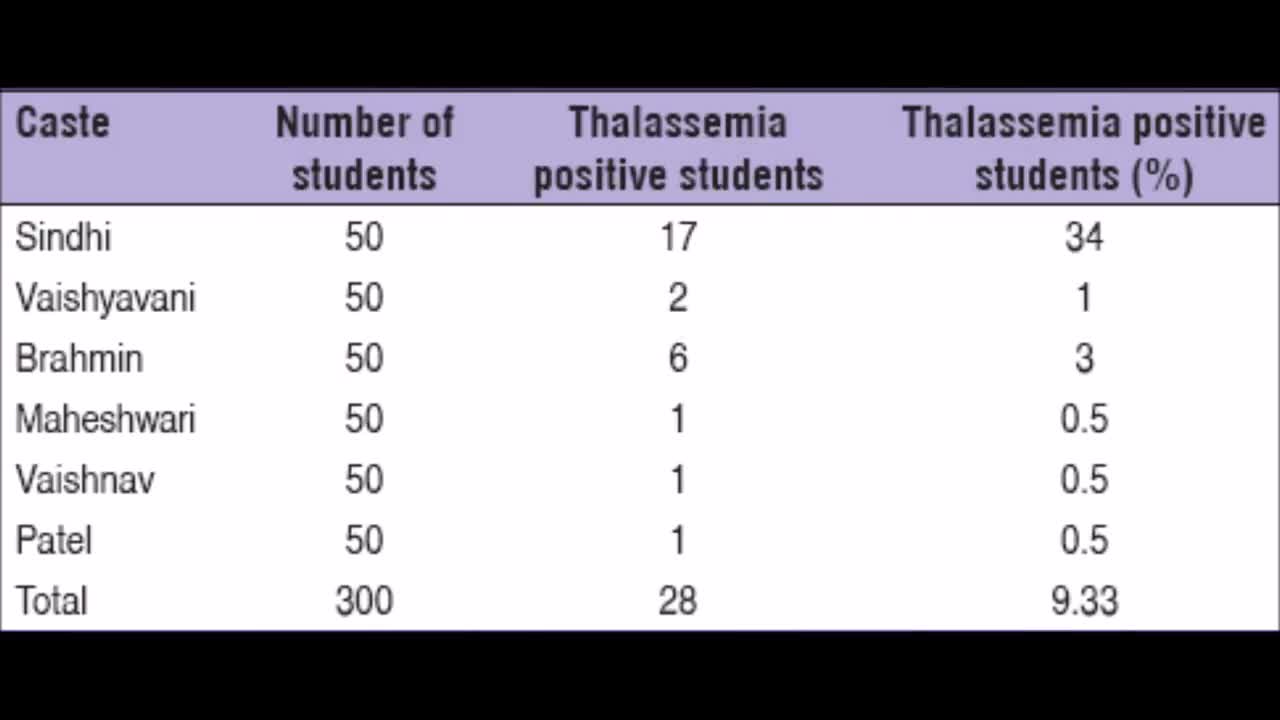
Thalassemia is a genetic blood disorder. People with Thalassemia disease are not able to make enough hemoglobin, which causes severe anemia. Hemoglobin is found in red blood cells and carries oxygen to all parts of the body. When there is not enough hemoglobin in the red blood cells, oxygen cannot get to all parts of the body. Organs then become starved for oxygen and are unable to function properly.
Pernicious anemia Email this page to a friend Print Facebook Twitter Google+ Anemia is a condition in which the body does not have enough healthy red blood cells. Red blood cells provide oxygen to body tissues. There are many types of anemia. Pernicious anemia is a decrease in red blood cells that occurs when the intestines cannot properly absorb vitamin B12.