Dernières vidéos
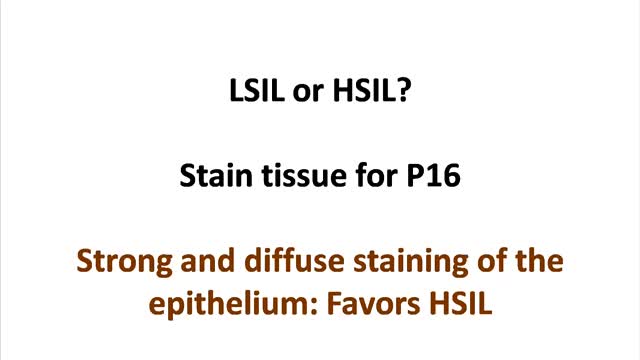
Cervical cancer occurs when abnormal cells on the cervix camera.gif grow out of control. The cervix is the lower part of the uterus that opens into the vagina. Cervical cancer can often be successfully treated when it's found early. It is usually found at a very early stage through a Pap test.
People with celiac disease may lose weight because their bodies are not able to absorb enough nutrients from food. Over time, a range of problems may develop as a result of the body's reaction to gluten — from skin rashes and lactose intolerance to infertility, bone weakness and nerve damage.
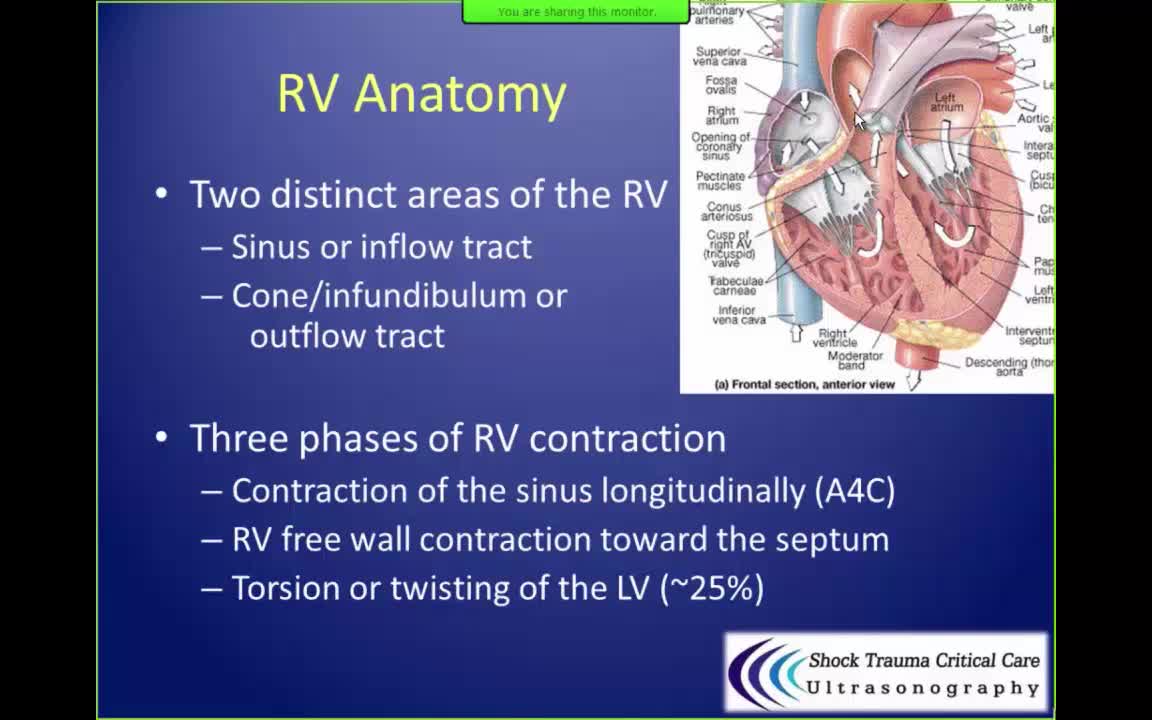
In patients with advanced congestive heart failure due to cardiomyopathy or ischemia, right ventricle shortening is the only significant independent associate of survival by multivariate analysis (as opposed to other parameters including left ventricular ejection fraction, cardiac index, and pulmonary resistance).

Microsurgical bipolar cautery tonsillectomy compares favorably with traditional techniques in terms of intraoperative bleeding, postoperative pain, otalgia, and hemorrhage. This technique combines the hemostatic advantage of cautery dissection, the excellent visualization achieved by a microscope, and, with the use of a video, greatly improves the physician's ability to teach how to perform a tonsillectomy.
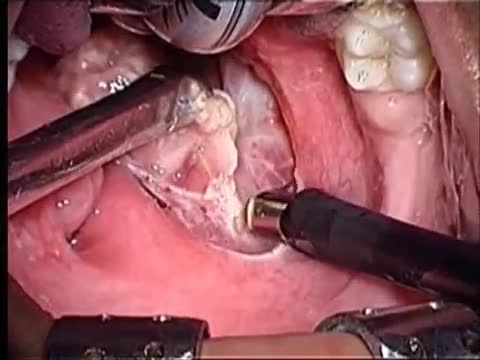
Tonsillectomy (ton-sih-LEK-tuh-me) is the surgical removal of the tonsils, two oval-shaped pads of tissue at the back of the throat — one tonsil on each side. A tonsillectomy was once a common procedure to treat infection and inflammation of the tonsils (tonsillitis). Today, a tonsillectomy is usually performed for sleep-disordered breathing but may still be a treatment when tonsillitis occurs frequently or doesn't respond to other treatments. A tonsillectomy may also be necessary to treat breathing and other problems related to enlarged tonsils and to treat rare diseases of the tonsils.

The cause for TS is unknown. Early research suggested that TS is an inherited condition (often, the person's near or distant relatives have had some form of transient or chronic tic disorder or associated symptoms). Recent studies point to a combination of environmental and genetic factors as a cause of the disorder. The specific genes involved in the development of TS are still being investigated. Studies suggest that TS has a neurological basis and results from an abnormality which affects the brain's metabolism of certain neurotransmitters (chemicals in the brain that regulate behavior.) Current research being funded by the Tourette Syndrome Association (TSA) will help provide more information about the causes and genetic factors of TS.
Most people with TS are not significantly impaired by their symptoms and therefore do not require treatment with medication. However, several medications are available to control TS symptoms that interfere with functioning. Except in more severe cases when tics are sometimes painful, the main reasons for medication are to improve appearance and lessen embarrassing social interactions. As with all medications, there are possible side effects that should be monitored carefully by the physician. Patients should always be included in the decision to take medication, as they are the best judge of how disruptive the symptoms are to them. Early diagnosis and treatment are crucial to help the person with TS cope with his or her condition. Often, people make fun of a person with TS. Parents of children with TS also may find it difficult to cope with their child's behavior. When people with TS are diagnosed correctly and treated for the condition early, they can learn to cope with their disorder and accept that they are ok and normal.

Psychological counseling can help parents learn to provide an appropriate environment for the child, especially for homework completion. Psychological counseling may also help children and their families deal more effectively with the social and emotional aspects of TS. Counseling can be an important part of treatment and should not be overlooked.

Tourette syndrome (also called Tourette's disorder or simply, "Tourette's") is an abnormal neurological condition characterized by motor and vocal tics. Tics are involuntary, rapid, sudden repetitive movements or sounds. Tics can be classified in a variety of ways. Motor tics can affect any part of the body including the head, neck, face, arms, shoulders, hands, feet, or legs. Facial tics, especially eye blinking, are usually the first symptoms of TS. Vocal tics are sounds that are made involuntarily. Vocal tics can include clearing the throat, coughing, sniffing, grunting, yelping, or shouting. In a few cases, vocal tics can include strange, inappropriate, or obscene words and phrases (called coprolalia). Vocal tics can also appear as constantly repeating the words of others (echolalia).

The da Vinci® Surgical System provides surgeons with an alternative to both traditional open surgery and conventional laparoscopy, putting a surgeon's hands at the controls of a state-of-the-art robotic platform. Our surgeons can perform even the most complex and delicate procedures through very small incisions with unmatched precision.

Shingles is a painful skin rash camera.gif. It is caused by the varicella zoster virus. Shingles usually appears in a band, a strip, or a small area on one side of the face or body. It is also called herpes zoster. Shingles is most common in older adults and people who have weak immune systems because of stress, injury, certain medicines, or other reasons. Most people who get shingles will get better and will not get it again. But it is possible to get shingles more than once.