Top videos
COMMON BLOOD DISORDERS
With bone marrow disease, there are problems with the stem cells or how they develop: In leukemia, a cancer of the blood, the bone marrow makes abnormal white blood cells. In aplastic anemia, the bone marrow doesn't make red blood cells. In myeloproliferative disorders, the bone marrow makes too many white blood cells.Nov 22, 2016
A bone marrow biopsy is part of a bone marrow test that takes a sample of your solid bone tissue. This test looks for abnormalities in your blood cells and signs of any diseases. You can request anesthesia or a sedative before the biopsy, and manage any pain afterward with over-the-counter medications.
Major signs and symptoms include enlargement of the liver and spleen (hepatosplenomegaly), a low number of red blood cells (anemia), easy bruising caused by a decrease in blood platelets (thrombocytopenia), lung disease, and bone abnormalities such as bone pain, fractures, and arthritis.
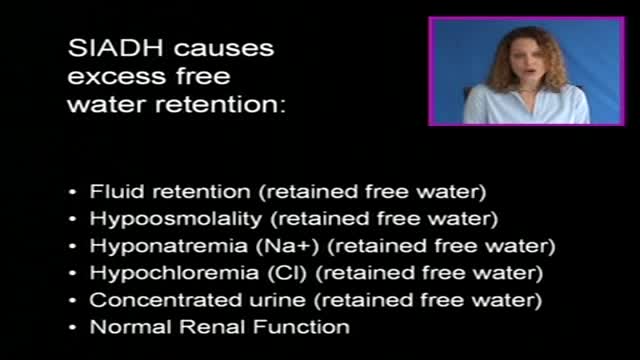
The syndrome of inappropriate antidiuretic hormone (ADH) secretion (SIADH) is defined by the hyponatremia and hypo-osmolality resulting from inappropriate, continued secretion or action of the hormone despite normal or increased plasma volume, which results in impaired water excretion.
Cushing's disease is a serious condition of an excess of the steroid hormone cortisol in the blood level caused by a pituitary tumor secreting adrenocorticotropic hormone (ACTH). ACTH is a hormone produced by the normal pituitary gland. ACTH stimulates the adrenal glands (located on top of the kidneys) to produce cortisol, commonly referred to as the stress hormone.
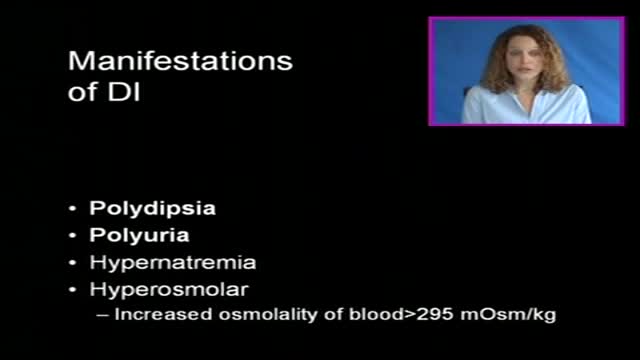
Diabetes insipidus (die-uh-BEE-teze in-SIP-uh-dus) is an uncommon disorder that causes an imbalance of water in the body. This imbalance leads to intense thirst even after drinking fluids (polydipsia), and excretion of large amounts of urine (polyuria). While the names diabetes insipidus and diabetes mellitus sound similar, they're not related. Diabetes mellitus — which can occur as type 1 or type 2 — is the more common form of diabetes. There's no cure for diabetes insipidus, but treatments are available to relieve your thirst and normalize your urine output.
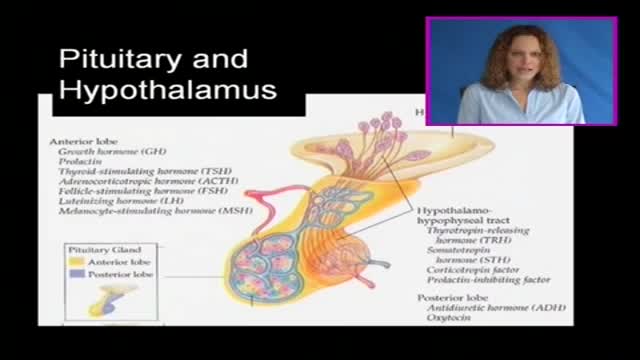
The pituitary gland is often portrayed as the "master gland" of the body. Such praise is justified in the sense that the anterior and posterior pituitary secrete a battery of hormones that collectively influence all cells and affect virtually all physiologic processes. The pituitary gland may be king, but the power behind the throne is clearly the hypothalamus. As alluded to in the last section, some of the neurons within the hypothalamus - neurosecretory neurons - secrete hormones that strictly control secretion of hormones from the anterior pituitary. The hypothalamic hormones are referred to as releasing hormones and inhibiting hormones, reflecting their influence on anterior pituitary hormones.
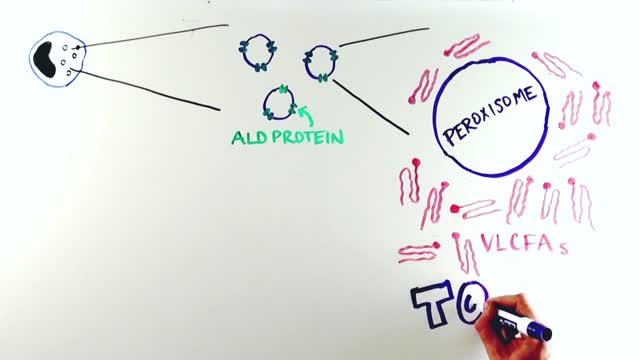
X-linked adrenoleukodystrophy is a genetic disorder that occurs primarily in males. It mainly affects the nervous system and the adrenal glands, which are small glands located on top of each kidney. In this disorder, the fatty covering (myelin) that insulates nerves in the brain and spinal cord is prone to deterioration (demyelination), which reduces the ability of the nerves to relay information to the brain. In addition, damage to the outer layer of the adrenal glands (adrenal cortex) causes a shortage of certain hormones (adrenocortical insufficiency). Adrenocortical insufficiency may cause weakness, weight loss, skin changes, vomiting, and coma.
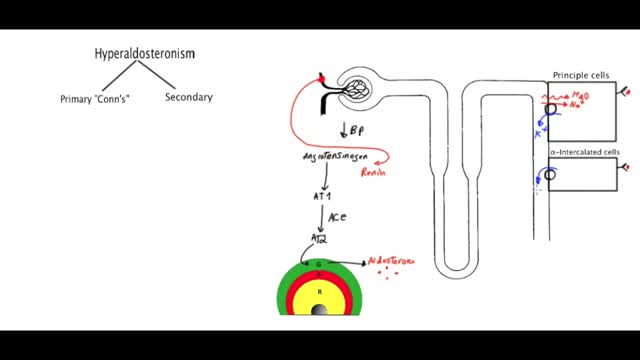
Primary aldosteronism, also known as primary hyperaldosteronism or Conn's syndrome, is excess production of the hormone aldosterone by the adrenal glands resulting in low renin levels. Often it produces few symptoms. Most people have high blood pressure which may cause poor vision or headaches.
Scoliosis is a sideways curvature of the spine that occurs most often during the growth spurt just before puberty. While scoliosis can be caused by conditions such as cerebral palsy and muscular dystrophy, the cause of most scoliosis is unknown.
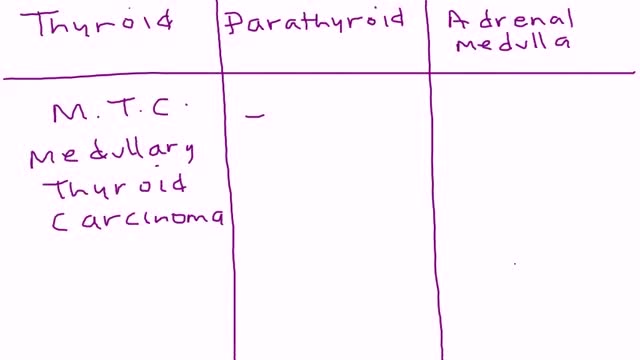
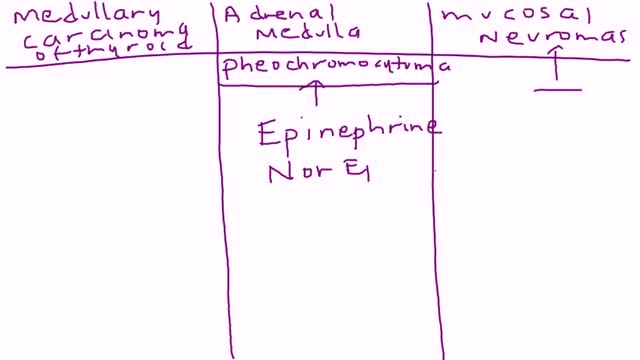
Multiple endocrine neoplasia type 2 (MEN2) (also known as "Pheochromocytoma and amyloid producing medullary thyroid carcinoma", "PTC syndrome," and "Sipple syndrome") is a group of medical disorders associated with tumors of the endocrine system. The tumors may be benign or malignant (cancer).
Multiple endocrine neoplasia type 2 (MEN2) is a hereditary condition associated with three primary types of tumors: medullary thyroid cancer, parathyroid tumors, and pheochromocytoma. MEN2 is classified into three subtypes based on clinical features. MEN2A, which affects 60% to 90% of MEN2 families Medullary thyroid cancer: 98% to 100% with MEN2A are affected Pheochromocytoma, a typically benign (noncancerous) tumor of the adrenal glands: 50% with MEN2A affected Parathyroid adenoma (benign tumor) or hyperplasia, meaning increased size, of the parathyroid gland: 5% to 10% with MEN2A affected MEN2B, which affects 5% of MEN2 families Medullary thyroid cancer: 98% to 100% with MEN2B affected Pheochromocytoma: 50% with MEN2B affected Mucosal neuromas, which is a benign tumor of nerve tissue on the tongue, lips and throughout the gastrointestinal tract: 95% to 98% affected Digestive problems caused by disordered nerves in the gastrointestinal tract: 75% to 90% affected Muscle, joint, and spinal problems: 95% affected Typical facial features, including swollen lips and thick eyelids: 75% to 90% affected Familial medullary thyroid cancer (FMTC), which affects 5% to 35% of MEN2 families Medullary thyroid carcinoma only Sources: Gagel RF, Marx SJ. “Multiple endocrine neoplasia.” Williams Textbook of Endocrinology, Chapter 40, 11th ed., Philadelphia, 2008, and Eng C, Clayton D, et al. Grubbs EG, Gagel RF. My, How Things Have Changed in Multiple Endocrine Neoplasia Type 2A! J Clin Endocrinol Metab 100(7):2532-5, 7/2015. PMID: 26151398. What causes MEN2? MEN2 is a genetic condition. This means that the cancer risk and other features of MEN2 can be passed from generation to generation in a family. The gene associated with MEN2 is called RET. A mutation (alteration) in the RET gene gives a person an increased risk of developing medullary thyroid cancer and other tumors associated with MEN2.
Parathyroid cancer is a rare disease in which malignant (cancer) cells form in the tissues of a parathyroid gland. The parathyroid glands are four pea-sized organs found in the neck near the thyroid gland. The parathyroid glands make parathyroid hormone (PTH or parathormone). PTH helps the body use and store calcium to keep the calcium in the blood at normal levels.
Euthyroid sick syndrome (ESS), sick euthyroid syndrome (SES), thyroid allostasis in critical illness, tumours, uremia and starvation (TACITUS), non-thyroidal illness syndrome (NTIS) or low T3 low T4 syndrome is a state of adaptation or dysregulation of thyrotropic feedback control where the levels of T3 and/or T4 are ...
NTIS refers to a syndrome found in seriously ill or starving patients with low fT3, usually elevated RT3, normal or low TSH, and if prolonged, low fT4. It is found in a high proportion of patients in the ICU setting, and correlates with a poor prognosis if TT4 is <4ug/dl. The patho-physiology includes suppression of TRH release, reducedT3 and T4 turnover, reduction in liver generation of T3, increased formation of RT3, and tissue specific down-regulation of deiodinases, transporters, and TH receptors. Although long debated, tissue TH levels are definitely reduced, and tissue hypothyroidism is presumably present. This is often not clinically evident because of the brief duration, and reduced but not absent tissue levels of TH. Although recognized for nearly 4 decades, interpretation of the syndrome is contested, because of lack of data. Some observes, totally without data, argue that it is a protective response and should not be treated. Other observers (as in this review) present available data suggesting, but not proving, that thyroid hormone replacement is appropriate, not harmful, and may be beneficial. The best form of treatment (TRH,TSH,or T3+T4) and possible accompanying treatments (GHRH, Cortisol, nutrition, insulin) lack consensus. In this review current data are laid out for reader’s review and judgment.
Diabetic retinopathy involves changes to retinal blood vessels that can cause them to bleed or leak fluid, distorting vision. Diabetic retinopathy is the most common cause of vision loss among people with diabetes and a leading cause of blindness among working-age adults.
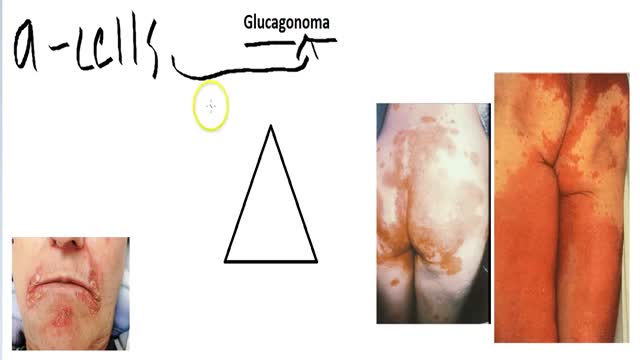
A glucagonoma is a rare tumor of the alpha cells of the pancreas that results in the overproduction of the hormone glucagon. Alpha cell tumors are commonly associated with glucagonoma syndrome, though similar symptoms are present in cases of pseudoglucagonoma syndrome in the absence of a glucagon-secreting tumor.
Diabetic retinopathy is classified into two types: Non-proliferative diabetic retinopathy (NPDR) is the early stage of the disease in which symptoms will be mild or nonexistent. In NPDR, the blood vessels in the retina are weakened. ... Proliferative diabetic retinopathy (PDR) is the more advanced form of the disease.
The vast majority of glucocorticoid activity in most mammals is from cortisol, also known as hydrocortisone. Corticosterone, the major glucocorticoid in rodents, is another glucocorticoid. Cortisol binds to the glucocorticoid receptor in the cytoplasm and the hormone-receptor complex is then translocated into the nucleus, where it binds to its DNA response element and modulates transcription from a battery of genes, leading to changes in the cell's phenotype. Only about 10% of circulating cortisol is free. The remaining majority circulates bound to plasma proteins, particularly corticosteroid-binding globulin (transcortin). This protein binding likely decreases the metabolic clearance rate of glucocorticoids and, because the bound steroid is not biologically active, tends to act as a buffer and blunt wild fluctuations in cortisol concentration.