Top video's
Routine pelvic exams are important for good reproductive health. A woman should have her first GYN exam when she first thinks about becoming sexually active, when she becomes sexually active or when she turns 18.
At the gynecologist, you will have a short general physical exam, including a breast exam. You will wear a hospital gown and nothing else. For the actual pelvic examination, you will lie down on an examination table with your feet resting in elevated “stirrups” (props that support your legs in the air). Stirrups might look a little scary, but they are there to keep you comfortable. Your legs will be spread apart, with your knees falling to each side so that your vagina is exposed. You may feel uncomfortable, but relax and realize that everyone goes through this.
External Exam
The practitioner will visually examine your vulva for discoloration, irritation, swelling and other abnormalities, and will gently feel for glands.
Internal Exam
There are two parts to the internal exam. The first involves a speculum, a metal or plastic instrument that the practitioner inserts into the vagina. The speculum is shaped like a duck’s bill, and once it is inserted into the vaginal canal, it is gently widened to spread the interior vaginal walls (this is not painful). As the vaginal walls are spread, the practitioner is able to see the walls of the vagina itself, and up the vaginal canal to the cervix. When viewing the vaginal canal and the cervix, the practitioner can look for discoloration, abnormal discharge, lesions, growths and signs of infection. It is possible for you to look at your own cervix during this process by propping yourself up on your elbows and using a mirror. Some practitioners ask if you would like to do this, but feel free to ask to if she doesn’t mention it first.
Pap Smear
Next the practitioner will take a pap smear. She/he uses a long-stemmed cotton swab to collect a sample of cells in the cervix. Some women feel a slight cramping sensation when their cervix is touched. The collected cells are smeared onto a slide and sent to a lab for testing and examination. The pap smear is extremely important for spotting abnormalities in the cervix which may indicate infection or disease.
STD Testing
If you are sexually active, the practitioner will test for STDs. The gynecologist will swab the inside of the cervix with a long cotton swab. The speculum is then taken out of the vagina. The samples are sent to a laboratory for various STD testing. The tests will probably take a couple days. Ask when your results will be available so you can call. If you want to be tested for HIV, syphilis, genital herpes or hepatitis you need to have blood taken. They can do that as well, but you will need to ask since it is not usually routine.
Manual Exam
The second part of the pelvic exam is called the manual or bi-manual exam. The practitioner will insert one or two fingers into your vagina and press with her/his other hand on the outside of your lower abdomen. They will use a lubricant on their fingers so it is more comfortable. The person can then feel the uterus, fallopian tubes and ovaries, and check for any swelling or tenderness. Once the doctor is finished checking your uterus and ovaries, the exam is complete. The entire pelvic exam (the parts involving your vagina, cervix, uterus, and ovaries) takes 3 to 5 minutes to complete.
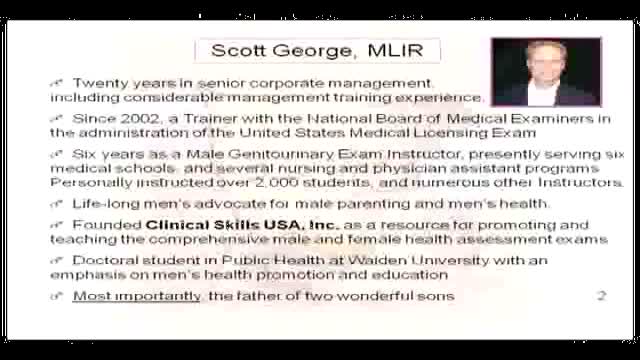
Physical exam by a urologist including kidney, testicular and prostate exam.
Traditional African treatment for infertility
http://www.proctoscopeexam.com This is a demonstration of a proctoscope examination of the rectum.
Tummy-tuck surgery or abdominoplasty, can flatten your abdomen by removing loose, excess fat and skin and tightening muscles in the abdominal wall. It can also remove some if not all of the stretch marks in your lower abdomen. It is popular following pregnancy, massive weight loss or whenever a flabby abdomen with weak muscles impairs body contour. Most patients report improved self-esteem as a result of this procedure.
A video showing the steps of cesarean section surgery
For those that aren't good LASIK candidates, PRK is a procedure that offers the same great results! Watch Dr. Ferguson explain each step during Samantha's procedure. Her reaction at the end is incredible!
Basic well-male examination of the genitals and digital rectal exam.
Dr Chris Steele demonstrates a breast examination on a live model. This shows how to check yourself for early signs of tumours, cysts and other symptoms of breast cancer.
Sciatic Nerve Block
LCHI - Hernia repair done by medical students with guidance and assistance of Professor Luiz Eduardo C. Miranda. Description of surgery is in portuguese.
Inguinal hernia Diagram of an indirect, scrotal inguinal hernia ( median view from the left). Diagram of an indirect, scrotal inguinal hernia ( median view from the left). By far the most common hernias (up to 75% of all abdominal hernias) are the so-called inguinal hernias. For a thorough understanding of inguinal hernias, much insight is needed in the anatomy of the inguinal canal. Inguinal hernias are further divided into the more common indirect inguinal hernia (2/3, depicted here), in which the inguinal canal is entered via a congenital weakness at its entrance (the internal inguinal ring), and the direct inguinal hernia type (1/3), where the hernia contents push through a weak spot in the back wall of the inguinal canal. Inguinal hernias are more common in men than women while femoral hernias are more common in women.
Orgasmic childbirth is a new variant of water birth delivery.
Aurogra 100mg is an oral tablet used to treat erection disorders in men. Aurogra is utilized to analyze erectile dysfunction in men, characterized as the powerlessness to get or keep a penile erection expected for sensual performance.
Buy Now : https://www.rsmenterprises.in/....product/viewdetail/a
#rsmenterprises #health #healthcare #aurogra100mg #sildenafil100mg #genericviagra #maleviagra
http://www.hypodermic-injection.com This is a demonstration of an IM hypodermic injection administered in the gluteus maximus muscle. The patient is in the prone position.
Peritoneal Dialysis for Kidney Disease
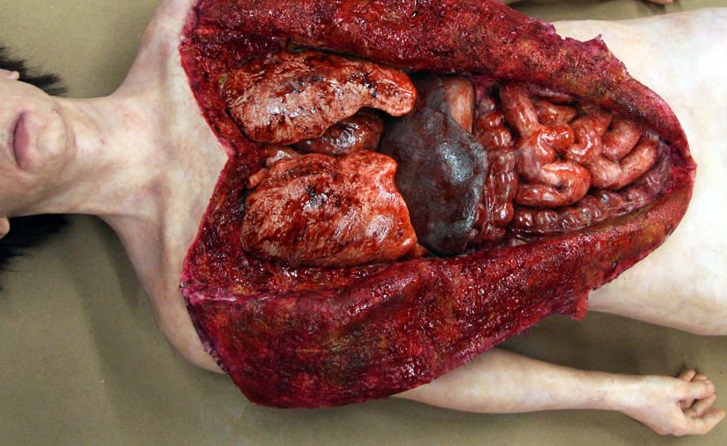
Watch that Full Female Body Medical Anatomy Autopsy
Child birth in squatting positions. The most comfortable position for the mother
A video showing the circumcision of a male baby
At Hutzel Women's Hospital, Dr. Giancarlo Mari performs breakthrough in-utero surgery to save the lives of high-risk twins developing with a rare "shared" circulatory problem. ~ Detroit Medical Center