トップ動画

Kneecap dislocation Email this page to a friend Print Facebook Twitter Google+ Kneecap dislocation occurs when the triangle-shaped bone covering the knee (patella) moves or slides out of place. The problem usually occurs toward the outside of the leg. Causes Kneecap (patella) dislocation is often seen in women. It usually occurs after a sudden change in direction when your leg is planted. This puts your kneecap under stress.

Lipomas are slow-growing soft tissue tumours that rarely reach a size larger than 2 cm. Lesions larger than 5 cm, so-called giant lipomas, can occur anywhere in the body but are seldom found in the upper extremities. The authors present their experiences with eight patients having giant lipomas of the upper extremity. In addition, a review of the literature, and a discussion of the appropriate evaluation and management are included.
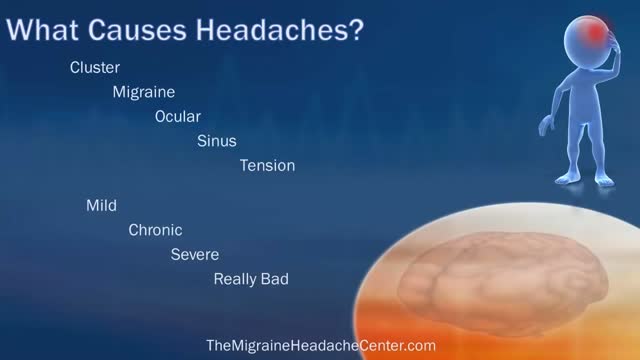
Your headache symptoms can help your doctor determine its cause and the appropriate treatment. Most headaches aren't the result of a serious illness, but some may result from a life-threatening condition requiring emergency care. Headaches are generally classified by cause: Primary headaches A primary headache is caused by overactivity of or problems with pain-sensitive structures in your head. A primary headache isn't a symptom of an underlying disease. Chemical activity in your brain, the nerves or blood vessels surrounding your skull, or the muscles of your head and neck (or some combination of these factors) can play a role in primary headaches. Some people may also carry genes that make them more likely to develop such headaches. The most common primary headaches are: Cluster headache Migraine (with and without aura) Tension headache (also known as tension-type headache) Trigeminal autonomic cephalalgia (TAC), such as cluster headache and paroxysmal hemicrania A few headache patterns also are generally considered types of primary headache, but are less common. These headaches have distinct features, such as an unusual duration or pain associated with a certain activity. Although generally considered primary, each could be a symptom of an underlying disease. They include: Chronic daily headaches (for example, chronic migraine, chronic tension-type headache, or hemicranias continua) Cough headaches Exercise headaches Sex headaches Some primary headaches can be triggered by lifestyle factors, including: Alcohol, particularly red wine Certain foods, such as processed meats that contain nitrates Changes in sleep or lack of sleep Poor posture Skipped meals Stress Secondary headaches A secondary headache is a symptom of a disease that can activate the pain-sensitive nerves of the head. Any number of conditions — varying greatly in severity — may cause secondary headaches. Possible causes of secondary headaches include: Acute sinusitis Arterial tears (carotid or vertebral dissections) Blood clot (venous thrombosis) within the brain — separate from stroke Brain aneurysm (a bulge in an artery in your brain) Brain AVM (brain arteriovenous malformation) — an abnormal formation of brain blood vessels Brain tumor Carbon monoxide poisoning Chiari malformation (structural problem at the base of your skull) Concussion Dehydration Dental problems Ear infection (middle ear) Encephalitis (brain inflammation) Giant cell arteritis (inflammation of the lining of the arteries) Glaucoma (acute angle closure glaucoma) Hangovers
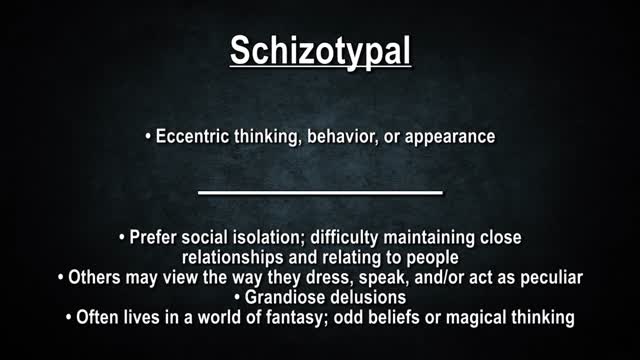
Personality disorders are a group of mental illnesses. They involve long-term patterns of thoughts and behaviors that are unhealthy and inflexible. The behaviors cause serious problems with relationships and work. People with personality disorders have trouble dealing with everyday stresses and problems. They often have stormy relationships with other people. The cause of personality disorders is unknown. However, genes and childhood experiences may play a role. The symptoms of each personality disorder are different. They can mild or severe. People with personality disorders may have trouble realizing that they have a problem. To them, their thoughts are normal, and they often blame others for their problems. They may try to get help because of their problems with relationships and work. Treatment usually includes talk therapy and sometimes medicine.

Emergency contraception is a method of birth control you can use if you had sex without using birth control or if your birth control method did not work correctly. You must use emergency contraception as soon as possible after unprotected sex. Emergency contraception pills are different from the abortion pill. If you are already pregnant, emergency contraception pills do not stop or harm your pregnancy. Emergency contraception has also been called the "morning-after pill," but you do not need to wait until the morning after unprotected sex to take it. Emergency contraception is not meant to be used for regular birth control. Talk to your doctor or nurse about regular birth control to help prevent pregnancy. Nearly half of all pregnancies in the United States are unplanned.1
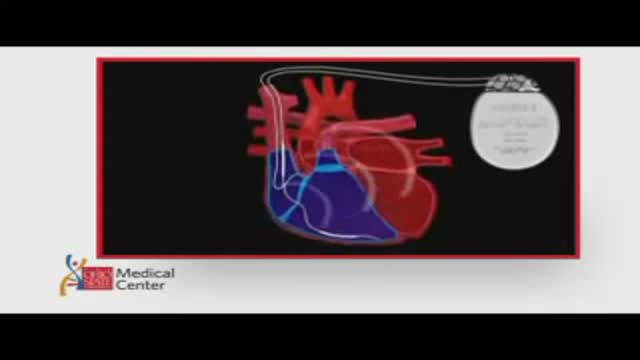
ICDs are useful in preventing sudden death in patients with known, sustained ventricular tachycardia or fibrillation. Studies have shown ICDs to have a role in preventing cardiac arrest in high-risk patients who haven't had, but are at risk for, life-threatening ventricular arrhythmias. View an animation of an ICD. Newer-generation ICDs may have a dual function which includes the ability to serve as a pacemaker. The pacemaker feature would stimulate the heart to beat if the heart rate is detected to be too slow. What is an Implantable Cardioverter Defibrillator (ICD)? An ICD is a battery-powered device placed under the skin that keeps track of your heart rate. Thin wires connect the ICD to your heart. If an abnormal heart rhythm is detected the device will deliver an electric shock to restore a normal heartbeat if your heart is beating chaotically and much too fast. ICDs have been very useful in preventing sudden death in patients with known, sustained ventricular tachycardia or fibrillation. Studies have shown that they may have a role in preventing cardiac arrest in high-risk patients who haven't had, but are at risk for, life-threatening ventricular arrhythmias.
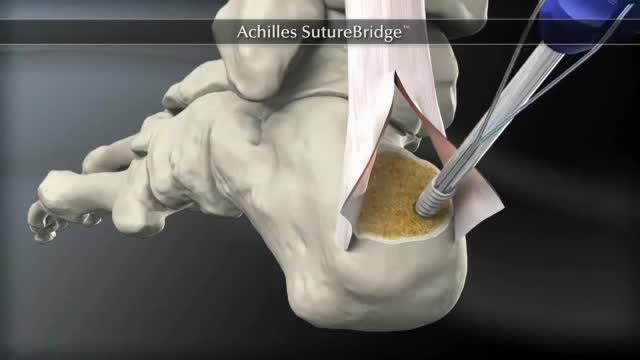
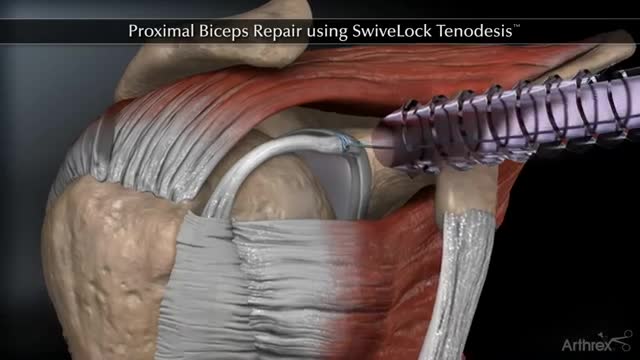
The Arthrex SpeedBridge™ is an innovative soft tissue fixation device used in the treatment of Achilles injuries. While standard anchor fixation of the tendon creates only a single point of compression directly over the anchor, the SpeedBridge enables an hourglass pattern of FiberTape® suture to be laid over the distal end of the tendon. This four-anchor construct enables a true knotless repair and a greater area of compression for the Achilles tendon on the calcaneus, improving stability and possibly allowing for earlier return to normal activities.
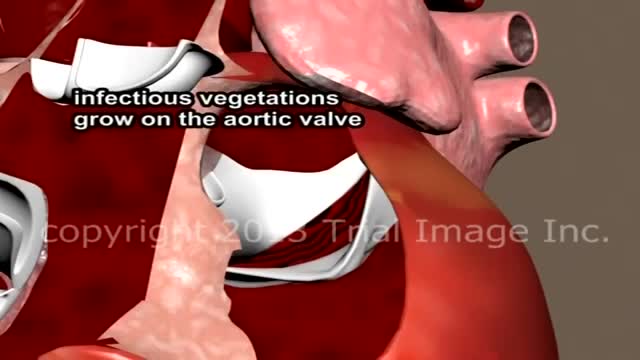
Endocarditis is an infection of the inner lining of your heart (endocardium). Endocarditis generally occurs when bacteria or other germs from another part of your body, such as your mouth, spread through your bloodstream and attach to damaged areas in your heart. Left untreated, endocarditis can damage or destroy your heart valves and can lead to life-threatening complications. Treatments for endocarditis include antibiotics and, in certain cases, surgery. Endocarditis is uncommon in people with healthy hearts. People at greatest risk of endocarditis have damaged heart valves, artificial heart valves or other heart defects.
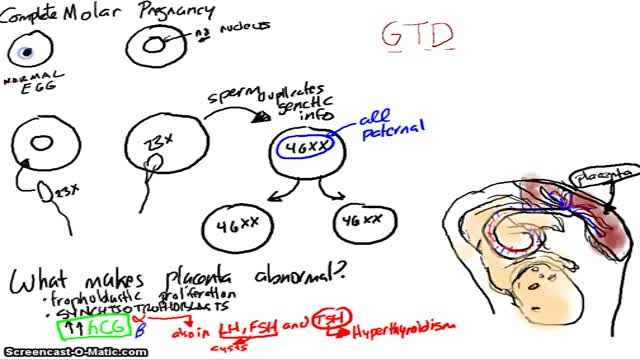
A molar pregnancy — also known as hydatidiform mole — is a noncancerous (benign) tumor that develops in the uterus. A molar pregnancy starts when an egg is fertilized, but instead of a normal, viable pregnancy resulting, the placenta develops into an abnormal mass of cysts. In a complete molar pregnancy, there's no embryo or normal placental tissue. In a partial molar pregnancy, there's an abnormal embryo and possibly some normal placental tissue. The embryo begins to develop but is malformed and can't survive. A molar pregnancy can have serious complications — including a rare form of cancer — and requires early treatment.

Bronchiolitis is a common lung infection in young children and infants. It causes inflammation and congestion in the small airways (bronchioles) of the lung. Bronchiolitis is almost always caused by a virus. Typically, the peak time for bronchiolitis is during the winter months. Bronchiolitis starts out with symptoms similar to those of a common cold but then progresses to coughing, wheezing and sometimes difficulty breathing. Symptoms of bronchiolitis can last for several days to weeks, even a month.
Appareil Pour La Cellulite, Creme Anti Cellulite Efficace, Anti Cellulite Maison, Café Cellulite--- http://perdre-sa-cellulite.plus101.com --- Cellulite Des Cuisses, Que Faire? Comment Eliminer Vite Sa Cellulite Des Cuisses Avec Des Exercices et L'alimentation cellulite-cuissesMême si la plupart des gens se mettent continuellement à la chasse de la cellulite, jusqu’à ce jour, il n’y a pas encore eu de remèdes miracles. Elle est particulièrement causée par le manque d’activités physiques et une alimentation non équilibrée. Elle apparaît souvent sur les fesses, les hanches et principalement sur les cuisses. Ainsi, pour se débarrasser de la cellulite surtout celle des cuisses, il est important d’avoir une alimentation équilibrée et de pratiquer des exercices sportifs. Il vous suffit de suivre les recommandations dans la vidéo ci-dessous qui vous aideront à tonifier vos jambes de manière efficaces, ainsi réduisant la présence de la cellulite sur les fesses, hanches et cuisses pour une silhouette plus attirante.CLIQUEZ ICI: http://perdre-sa-cellulite.plus101.com

LSD is one of the most potent, mood-changing chemicals. It is manufactured from lysergic acid, which is found in the ergot fungus that grows on rye and other grains. It is produced in crystal form in illegal laboratories, mainly in the United States. These crystals are converted to a liquid for distribution. It is odorless, colorless, and has a slightly bitter taste.

Wisdom teeth extractions can rear their ugly head later in life. This is a video of a patient with neck pain and neck weakness. When we stimulated the nerve fibers in the area of the extracted teeth there was an immediate improvement in her ability to control her neck muscles.