I migliori video

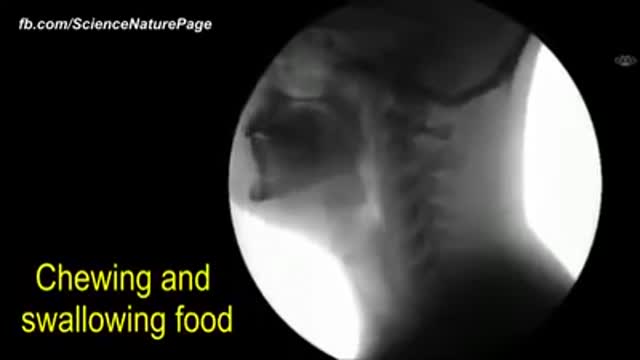
For education, Microsoft HoloLens will help make incredible leaps forward in productivity, collaboration, and innovation. See how Microsoft HoloLens transforms the way we teach anatomy and our understanding of the human body as we help to prepare the next generation of doctors.

Shaken baby syndrome — also known as abusive head trauma, shaken impact syndrome, inflicted head injury or whiplash shake syndrome — is a serious brain injury resulting from forcefully shaking an infant or toddler. Shaken baby syndrome destroys a child's brain cells and prevents his or her brain from getting enough oxygen. Shaken baby syndrome is a form of child abuse that can result in permanent brain damage or death. Shaken baby syndrome is preventable. Help is available for parents who are at risk of harming a child. Parents also can educate other caregivers about the dangers of shaken baby syndrome.
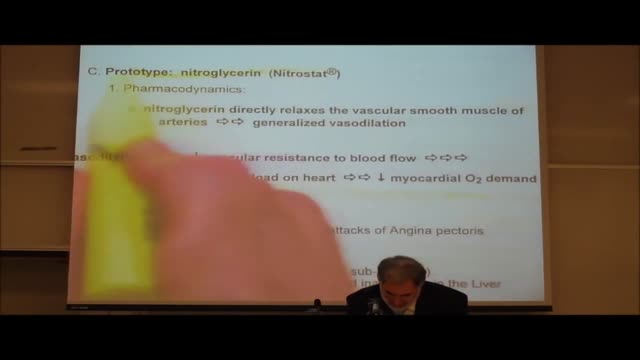
Angina results from a reduction in the oxygen supply/demand ratio. Therefore, in order to alleviate the pain, it is necessary to improve this ratio. This can be done either by increasing blood flow (which increases oxygen delivery or supply), or by decreasing oxygen demand (i.e., by decreasing myocardial oxygen consumption).

When a stroke affects an extensive portion of the front and back regions of the left hemisphere, the result may be global aphasia. Survivors with global aphasia: May have great difficulty in understanding words and sentences. May have great difficulty in forming words and sentences. May understand some words. Get out a few words at a time. Have severe difficulties that prevent them from effectively communicating.

The hips are one of the hardest places to loose fat. Liposuction can be done on this area to dramatically help loose inches. This area is also one of the most successful areas to show visible improvement after liposuction is done. Liposuction of the hips can help patients to reduce dress and pant sizes. Disclaimer. The photographs on these pages illustrate typical results of some liposuction surgery procedures and may contain some nudity. Viewer discretion is advised. In providing the photos and statements on this web site, Liposuction.com does not state or imply any guarantee.

Beckwith-Wiedemann Syndrome (BWS) is a congenital overgrowth syndrome, which can affect all systems of the body. It was first recognised in 1963-64 by Dr J. Bruce Beckwith, a paediatric pathologist in America and, independently, by Dr H.E. Wiedemann, a German geneticist.
Diagnosis of HIV infection in infants is aided by HIV culture or DNA/RNA polymerase chain reaction (PCR); positive results are confirmed by repeating the test. In suspected cases, HIV testing should occur in the newborn period (ie, before the infant is 48 h old), at age 1-2 months, and again at age 3-6 months.

Mother-to-child transmission of HIV is the spread of HIV from an HIV-infected woman to her child during pregnancy, childbirth (also called labor and delivery), or breastfeeding (through breast milk). Mother-to-child transmission of HIV is also called perinatal transmission of HIV.

Wetness. Even the most absorbent diaper leaves some moisture on your child's skin. And when your child's urine mixes with bacteria from his stool, it breaks down into ammonia, which can be very harsh on the skin. That's why children with frequent bowel movements or diarrhea are more prone to diaper rash.

LSD is one of the most potent, mood-changing chemicals. It is manufactured from lysergic acid, which is found in the ergot fungus that grows on rye and other grains. It is produced in crystal form in illegal laboratories, mainly in the United States. These crystals are converted to a liquid for distribution. It is odorless, colorless, and has a slightly bitter taste.