Top videos

Runners Knee Overview:
Welcome to our Patello-Femoral Rehab video. The goal of this video is to minimize pain around the kneecap and maximize recovery. This video should not be used as a substitute for regular physical therapy visits and guidance from your physician
Visit http://www.matthewboesmd.com/p....atello-femoral-rehab for more information

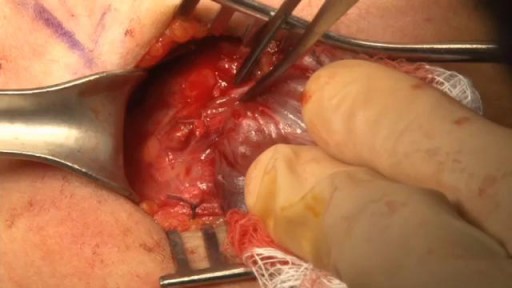
Traditionally, the appendix is removed through an incision in the right lower abdominal wall. In most laparoscopic appendectomies, surgeons operate through 3 small incisions (each ¼ to ½ inch) while watching an enlarged image of the patient's internal organs on a television monitor.

Get our Knee Resilience Program here: https://store.e3rehab.com/products/knee-resilience
👟 Vivo Barefoot: Get 15% off all shoes! - https://www.vivobarefoot.com/e3rehab
What is patellofemoral pain, also referred to as runner’s knee? Check out the video to find out!
Want to watch more? Check out our full video: https://youtu.be/K3HxB6rAeDo?t
Subscribe to our channel and turn on notifications so you don't miss any videos: @E3Rehab
We are Doctors of Physical Therapy who specialize in rehabilitation, pain, performance, and injury risk reduction. Our mission is simple: empower YOU to overcome your setbacks and crush your goals using evidence-based education. For more info, check out: https://e3rehab.com/
More videos: https://www.youtube.com/@E3Rehab/videos
Podcast: https://open.spotify.com/show/....5ZbaI145Bk94Guq7olMJ
Instagram: https://www.instagram.com/e3rehab/
Twitter: https://twitter.com/E3Rehab
---
Disclaimer: The information presented is not intended as medical advice or to be a substitute for medical counseling but is intended for entertainment purposes only. If you are experiencing pain, please seek the appropriate healthcare professional.

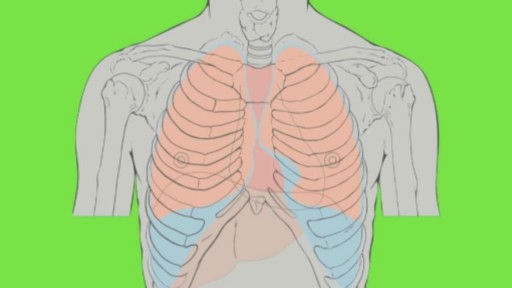
This 3D animation video explains airway clearance anatomy & physiology in the lungs.
Learn more about Baxter Respiratory Health products at www.hillrom.com/en/products-ca....tegory/non-invasive-
Rx Only. For safe and proper use of product mentioned herein, please refer to the Instructions for Use or Operator manual.
The information contained in these videos is provided for educational purposes only and is not intended nor implied to be a substitute for professional medical advice. You assume full responsibility for how you choose to use this information. Please speak with your healthcare provider about any questions you may have regarding a medical condition.
Baxter retains all right, title, and interest in and to the video, and retains the right to demand that you immediately cease use of the video and unembed the video. Baxter may discontinue or disable videos you have embedded at any time for any reason. You will not misrepresent the content contained in the video or use it in conjunction with price comparisons, in derogatory comparisons or in negative comparisons, with Baxter's competitor's products, or in derogatory or negative commentaries about Baxter's products - doing so may subject you to liability. Any and all claims made by you regarding the use, operation, quality, etc. of Baxter's products are your own, and you shall be responsible for ensuring that all such claims comply fully with all applicable federal, state and local laws.
US-FLC174-230024 v1

Iodine For Ringworm, Best Ointment For Ringworm, Where Do You Get Ringworm, How To Treat Ring Worms ---- http://ringworm-cure.plus101.com --- Ringworms, contrary to the common notion, do not come from worms. Tinea, which is the medical term for ringworms, is a fungal infection seen on the skin's surface. Knowing how to cure ringworm is important because ringworms can be highly contagious. It can be contracted from direct contact with the host (person or animal) as well as by other means such as having contact with the host's clothes. Swimming pools can also be a place where ringworms are transmitted from one person to another. How To Cure Ringworm - Understanding Aspects and Options Different means on how to cure ringworm are available and they sometimes vary in accordance with where the ringworm is located (it can appear in areas like the nails, fingers, toes, feet, scalp, stomach, chest, thighs, and scalp), and the particular type of ringworm. • Ringworms found in the scalp are usually treated with an antifungal shampoo to keep the area dry and clean. • Ringworms found in the feet can be treated through the application of ointments. • Oral medications can also be taken in especially when ringworms are on the nails. • Sprays, powders and creams are also forms by which anti-fungal drugs are bought. These medicines may take some time to work. The infection may persist for a few weeks to several months, depending on the severity and how the body responds to the medications. How To Cure Ringworm - OTC and Prescription Medications Ringworm appears on the skin's surface as an itchy, red, circular patch. As it progresses, it expands and smaller round patches can develop. It is important to immediately identify ringworms and know how to treat them properly. There are many over the counter topical creams (anti-fungal ones) and ointment that can be bought in the market. However, some people prefer to visit the doctor and ask for a prescription. Stronger formulations are generally available via prescriptions. William Oliver is a nutritionist, medical researcher, and author of the Fast Ringworm Cure e-book. To find out how to cure Ringworm in 3 days or less, click below: http://ringworm-cure.plus101.com
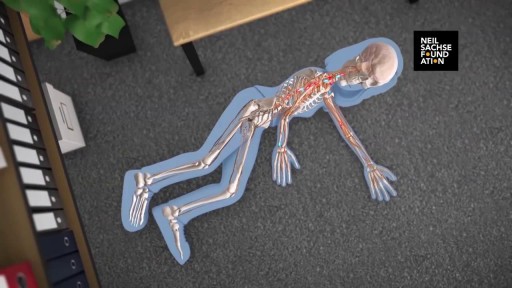
In multiple sclerosis, the immune system attacks the protective sheath called myelin, that covers nerve fibers and causes communication problems between your brain and the rest of your body. Eventually, the disease can cause the nerves to deteriorate or become damaged.
Boqueras Causas, Como Se Quitan Las Boqueras, Porque Salen Boqueras En La Boca, Queilitis Angular --- http://queilitis-angular.good-info.co --- Hay Que Actuar Ante Los Primeros Signos De Queilitis Angular. Las Primeras Manifestaciones De Queilitis Angular Suelen Ser Tenues Y Apenas Molestas. Pero No Por Ello Hay Que Ignorarlas, Porque Pueden Derivar En Problemas Mayores. La Queilitis Angular O Lo Que Comúnmente Se Llaman Boqueras, Comienza Por Grietas Minúsculas En Los Extremos De La Boca. También Se Empieza A Sentir Ardor Y Molestias Al Mover Los Labios O Al Abrir La Boca. ¿Qué Sucede Si No Se Atienden De Inmediato Esas Pequeñas Molestias? Difícilmente Se Irán Por Si Solas Sino Que, Por El Contrario, Comenzarán A Agravarse. Las Minúsculas Grietas Se Harán Cada Vez Más Pronunciadas Por El Continuo Movimiento De La Boca. Al Intensificarse Las Grietas Pueden Llegar A Convertirse En Llagas Y A Sangrar. Y Las Infecciones No Tardarán En Aparecer. La Queilitis Angular Puede Ser En Un Primer Momento Molesta Para Quien La Sufre. A Medida Que Avanza, Las Pequeñas Manifestaciones En La Boca Comienzan A Ser Bien Visibles Y Desagradables. Por Lo Que Al Ardor, Picazón Y Dolor, Se Le Suma El Hecho De Querer Ocultar La Afección Ante Los Demás. Cosa Que No Es Fácil De Lograr. A Pesar De Ser Pequeña, La Boca Es Uno De Los Lugares Más Visible Y Observado. Si Hablamos, Comemos, Bebemos, Nuestra Boca Está En Primer Plano. Ante Los Primeros Signos De Queilitis Se Puede Recurrir A Una Crema O Pomada Adecuada, Antiséptica, Antimicótica O Antifúngica. Si Bien Los Extremos De La Boca Deben Permanecer Libres De Saliva O Transpiración, Deben Estar Bien Hidratados. Cualquier Crema Antiséptica Que Se Utilice Debe Ser Libre De Perfumes Y Colorantes Químicos. Debe Detener La Descamación, A La Vez Que Calmar El Picor. El Área Afectada Tendrá Que Permanecer Bien Aseada, Procediendo A Secarla Sin Frotar, Como Para Que No Se Resienta Aún Más La Piel De Los Labios Y Sus Adyacencias. Para Curar La Queilitis Angular No Alcanza Con Los Tópicos Que Se Puedan Utilizar, Por Más Efectivas Que Sean Sus Fórmulas Desde Las Primeras Aplicaciones. Hay Que Llevar A Cabo Una Nutrición Balanceada, Variada Y Suficiente, Con Vitaminas, Minerales Y Oligoelementos. Un Análisis De Laboratorio Podrá Determinar Si Está Haciendo Falta El Aporte De Alguna Vitamina O Mineral. Asimismo, Conviene Evitar Los Lugares Muy Fríos Y/O Húmedos, Así Como Los Espacios Contaminados Por Polvillos O Cualquier Sustancia Irritante Para La Piel. Recomendamos Siempre Actuar Ante Los Primeros Síntomas De Queilitis. Si Se Frena La Dolencia Antes De Que Prospere Y Haga Eclosión, Se Evitará El Sufrimiento Que Puede Implicar Lidiar Contra Lesiones Serias En La Boca. Y Se Evitarán Las Temibles Huellas De Cicatrices Que Pueda Dejar Una Afección Prolongada. ¿Qué Podemos Hacer Ya Mismo? Hoy Existe Un Novedoso Tratamiento, Totalmente Natural Y Muy Simple, Con El Que Se Puede Eliminar La Queilitis Angular O Boqueras En Tan Solo 7 Días (O Menos). Este Revolucionario Sistema Ataca La Verdadera Causa De La Enfermedad Y No Solo Los Síntomas, Asegurando Resultados A Largo Plazo. Si Usted Desea Eliminar Para Siempre Esas Grietas Dolorosas Y La Vergüenza Que Causa Esta Afección, Puede Conocer Este Método De Resultados Comprobados Haciendo Clic En El Siguiente Enlace http://queilitis-angular.good-info.co

Common Medicines For General Medical Practice / Medicine Name and Uses
This Video Is For Medical Students,
In This Video We Are Talking About Most Commonly Used Medicine,
If You Like The Video, Be Sure To Subscribe To The Channel
More videos links.
How To Give Injection in Cannula Easily at Home
https://youtu.be/_KcpmGpE-dM
IV Drip Procedures in Hindi || IV Fluid Management
https://youtu.be/uz0Mecd4_3U
47 Basic Orthopedic Instruments Name And uses
https://youtu.be/i8i_B5XpmqQ
Common Medical Terms
https://youtu.be/2FsH61ZYTFE
Iv cannula,IV Cannula Colour Size external diameter and flow rate https://youtu.be/ijMlJ1KOgcU
38 Obstretice & Gynecology Instruments With Names And Their Uses https://youtu.be/xkx6wIFqmP0
C- Section All Instruments With Names And Uses
https://youtu.be/dwo2fXhKhW8
Appendectomy All Instruments With Names And Uses
https://youtu.be/B-J-0MQ4jZk
41 Basic Hospital Equipment with names and uses
https://youtu.be/U8tKeMLl5p4
42 Surgical instruments With Names And Uses
https://youtu.be/U8tKeMLl5p4
Abdominal surgery instruments With Names And Uses
https://youtu.be/sw__xDN0CQc
37 Basic Medical Equipments With Names And Uses
https://youtu.be/sw__xDN0CQ
________________________________________
#medicine
#medicines
#medicineinformation
#emergencyin
#emergency
#injection
#injection_video
#medical
#medicalstudent
#nursing
#nursingexam
#mbbs
#doctor
#doctors
#medicalstudentsmotivationvideo
Pulmonary edema is usually caused by a heart condition. Other causes include pneumonia, exposure to certain toxins and drugs, and being at high elevations. Depending on the cause, pulmonary edema symptoms may appear suddenly or develop over time. Mild to extreme breathing difficulty can occur. Cough, chest pain, and fatigue are other symptoms. Treatment generally includes supplemental oxygen and medications.

Swelling is a typical symptom of lymphedema and commonly affects legs and arms. Compression stockings work to encourage the movement of lymph out of an affected limb. Lymphedema is incurable. However, treatment can help reduce the swelling and pain

Prompt treatment to break up the clot greatly reduces the risk of death. This can be done with blood thinners and drugs or procedures. Compression stockings and physical activity can help prevent clots from forming in the first place.

Dr. Nick demonstrates how easy it is to have stitches taken out and that it is not painful!
#shorts #satisfying #reaction
 MAKE SURE TO SUBSCRIBE FOR ALL THE NEW SURGICAL AND EDUCATIONAL VIDEOS COMING!!
👉🏻For more information visit :
https://drnickcampi.com
👉🏻Follow me on TikTok!!
https://vm.tiktok.com/ZMeXLbc5F/
👉🏻Connect with me!!
https://www.instagram.com/drnickcampitelli
👉🏻Check out this video of how we remove an ingrown toenail!
https://youtu.be/JyZo8aZDYds
👉🏻Dr. Nick Campitelli Performs latest Minimally Invasive Bunion Surgery! Watch this video!
https://youtu.be/eRpABMsCbOU
Dr. Nick Campitelli is a podiatrist who specializes in foot and ankle surgery in the Akron and Cleveland Ohio area. He is the Residency Director of the Western Reserve Hospital / University Hospital Podiatric Medicine and Surgery Residency Program.
*** All content found on the this YouTube video including: text, images, audio, or other formats were created for informational purposes only. The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you heard on this video. ***

Many people have baggy and puffy lower eyelids. Lower Eyelid Surgery (Blepharoplasty) is the removal of excess fat and tightening of the skin, which can drastically minimize the appearance of baggy and puffy lower eyelids that makes everyone look tired and worn down. This procedure is just as popular with men as with women. A sense of well-being and alertness is the reason why most people elect to have this procedure. Lower lids surgery is a procedure that the best results are achieved when performed earlier than later. Dr. Lee has performed this surgery on patients who are 18 yrs old to 82 yrs old- all very happy with their results. The cause of baggy and puffy lower eyelid is due to a combination of herniating fat, excessive skin, and edema (water retention).