Top videos
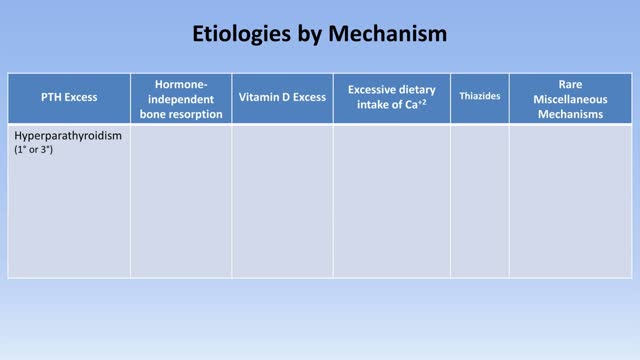
Hypercalcemia is a condition in which the calcium level in your blood is above normal. Too much calcium in your blood can weaken your bones, create kidney stones, and interfere with the way your heart and brain works. Hypercalcemia most commonly results from overactive parathyroid glands. These four tiny glands are each about the size of a grain of rice and are located on or near the thyroid gland. Other causes of hypercalcemia include cancer, certain other medical disorders, some medications, and excessive use of calcium and vitamin D supplements. Signs and symptoms of hypercalcemia may range from nonexistent to severe. Treatment depends on the underlying cause.
The exact cause of schizophrenia isn't known, but genetics, environment, and imbalanced brain chemicals may play a role. Schizophrenia is characterized by abnormal social behavior. In severe cases, patients may see or hear things that aren't real. Treatment is usually lifelong and often involves a combination of medications and psychological and social therapy.
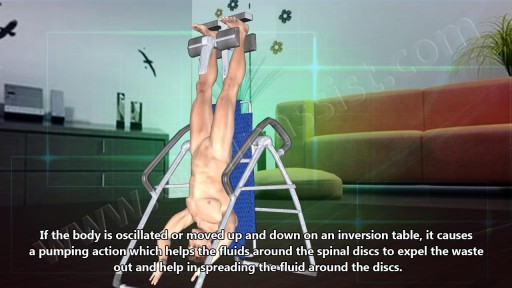
Many people report that inversion table therapy is a great way to stretch muscles and ligaments, reduce muscle spasms, and improve circulation. Stretching stimulates the lymph glands to increase the flow of lymphatic fluids; part of the body's waste disposal system. Similarly, cellular health depends on good blood circulation to deliver nourishment and remove waste. Inversion table therapy also helps to relieve motion sickness and stress. In addition, the body becomes more aware of its spatial orientation and balance when the inner ear is stimulated during inversion. Plus, it is not necessary for the body to be positioned completely upside down to gain benefits from inversion therapy! Unlike antigravity boots used with an inversion rack, an adjustable inversion table offers the flexibility to choose the most comfortable angle. Dialogue with Your Doctor Like anything that can affect your health, talk to your doctor before you start using an inversion table. This is important because certain medications and health conditions may make using an inversion table unsafe. Your doctor may recommend against inversion table therapy if you have obesity, a detached retina, fracture, glaucoma, heart condition (circulatory problem), hernia, implanted device, middle ear or eye infection, osteoporosis, are pregnant, or have a spinal injury. There may be other medical conditions not listed that your doctor may view as a contraindication.

Preeclampsia is a pregnancy complication characterized by high blood pressure and signs of damage to another organ system, often the kidneys. Preeclampsia usually begins after 20 weeks of pregnancy in a woman whose blood pressure had been normal. Even a slight rise in blood pressure may be a sign of preeclampsia. Left untreated, preeclampsia can lead to serious — even fatal — complications for both you and your baby. If you have preeclampsia, the only cure is delivery of your baby. If you're diagnosed with preeclampsia too early in your pregnancy to deliver your baby, you and your doctor face a challenging task. Your baby needs more time to mature, but you need to avoid putting yourself or your baby at risk of serious complications.

This video will cover, in detail, the motor, sensory, reflect components of a neurological examination.
This video is created for the UBC Medicine Neurology Clinical Skills curriculum as part of MEDD 419 FLEX projects.
Filmed, written, and directed by:
John Liu
Vincent Soh
Chris Calvin
Kashi (Siyoung) Lee
Kero (Yue) Yuen
Ge Shi
Doctor - Dr. Jason Valerio (Department of Neurology, UBC)
Supervised by:
Dr. Alex Henri-Bhargava (Department of Neurology, UBC)
Zac Rothman (UBC FOM Digital Solutions: Ed Tech)
Edited by:
Stephen Gillis
Produced by UBC FOM Digital Solutions EdTech team facilitates innovation by UBC Medicine learners and faculty.
Website: https://education.med.ubc.ca/
Subscribe: https://www.youtube.com/ubcmed....vid?sub_confirmation
UBCMLN Podcast Network: https://tinyurl.com/ubcmedicinelearningnetwork
----------------------------------------------------------------------------------------------------------------------------------------------------------
The Vancouver Fraser Medical Program and the Vancouver Academic Campus of the University of British Columbia are situated on the traditional territory of the Musqueam, Squamish and Tsleil-Waututh peoples.
The Southern Medical Program and the Okanagan Academic Campus of the University of British Columbia are situated on the territory of the Syilx Okanagan Nation.
The Northern Medical Program and the University of Northern BC are situated on the traditional territory of the Lheidli T’enneh, part of the Dakelh (Carrier) First Nations.
With respect the Lekwungen peoples on whose traditional territory the Island Medical Program and the University of Victoria stand and the Songhees, Esquimalt and WSÁNEĆ peoples whose historical relationships with the land continue to this day.
We acknowledge our traditional hosts and honour their welcome and graciousness to the students who seek knowledge here.
© UBC Faculty of Medicine
All rights reserved. Reproduction and distribution of this presentation without written permission from UBC Faculty of Medicine is strictly prohibited.

Most of the time when someone with cancer is told they have cancer in the bones, the doctor is talking about a cancer that has spread to the bones from somewhere else. This is called metastatic cancer. It can be seen in many different types of advanced cancer, like breast cancer, prostate cancer, and lung cancer. When these cancers in the bone are looked at under a microscope, they look like the tissue they came from. For example, if someone has lung cancer that has spread to bone, the cells of the cancer in the bone still look and act like lung cancer cells. They do not look or act like bone cancer cells, even though they are in the bones. Since these cancer cells still act like lung cancer cells, they still need to be treated with drugs that are used for lung cancer. For more information about metastatic bone cancer, please see our document called Bone Metastasis, as well as the document on the specific place the cancer started (Breast Cancer, Lung Cancer, Prostate Cancer, etc.). Other kinds of cancers that are sometimes called “bone cancers” start in the blood forming cells of the bone marrow − not in the bone itself. The most common cancer that starts in the bone marrow and causes bone tumors is called multiple myeloma. Another cancer that starts in the bone marrow is leukemia, but it is generally considered a blood cancer rather than a bone cancer. Sometimes lymphomas, which more often start in lymph nodes, can start in bone marrow. Multiple myeloma, lymphoma, and leukemia are not discussed in this document. For more information on these cancers, refer to the individual document for each. A primary bone tumor starts in the bone itself. True (or primary) bone cancers are called sarcomas. Sarcomas are cancers that start in bone, muscle, fibrous tissue, blood vessels, fat tissue, as well as some other tissues. They can develop anywhere in the body. There are several different types of bone tumors. Their names are based on the area of bone or surrounding tissue that is affected and the kind of cells forming the tumor. Some primary bone tumors are benign (not cancerous), and others are malignant (cancerous). Most bone cancers are sarcomas.

This video shows you how to conduct a clinical examination of the foot and how to identify common causes of foot pain.
This video clip is part of the FIFA Diploma in Football Medicine and the FIFA Medical Network. To enrol or to find our more click on the following link http://www.fifamedicalnetwork.com
The Diploma is a free online course designed to help clinicians learn how to diagnose and manage common football-related injuries and illnesses. There are a total of 42 modules created by football medicine experts. Visit a single page, complete individual modules or finish the entire course.
The network provides the opportunity for clinicians around the world to meet and share ideas relating to football medicine. Ask about an interesting case, debate current practice and discuss treatment strategies. Create a profile and log on to interact with other health professionals from around the globe.
This is not medical advice. The content is intended as educational content for health care professionals and students. If you are a patient, seek care of a health care professional.

Visit our website to learn more about using Nucleus animations for patient engagement and content marketing: http://www.nucleushealth.com/?utm_source=youtube&utm_medium=video-description&utm_campaign=appendect-020615
This 3D medical animation depicts the surgical removal of the appendix (appendectomy) using laparoscopic instruments. The surgery animation begins by showing an inflamed appendix (appendicitis), followed by the placement of the laparoscope. Afterward, one can see the surgical device staple, cut and remove the inflamed appendix. Following the removal of the appendix the abdomen is flushed with a sterile saline solution to ensure all traces of infection have been removed.
#laparoscopy #appendix #appendicitis
ANCE00183

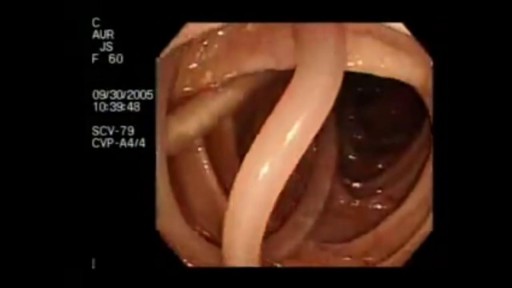
Experience with endoscopic retrograde cholangiopancreatography (ERCP) in children has been limited due to multiple factors, including the relatively low incidence of diseases requiring ERCP in this age group, the impression that the procedure is technically difficult in children, and because the indications and safety of ERCP in children have not been well defined. As a result, patients are generally referred to a tertiary care facility or to adult endoscopists who perform a high volume of procedures.