Top videos

Shoutout to director/videographer Valentina Vee and producer Sean Tien for helping me bring this to life.
New Comedy Show Dates!
SAN DIEGO, 8/26-8/27
LAS VEGAS, 9/3
HUNTINGTON BEACH, 9/9
WASHINGTON D.C., 10/7-10/8
Get Tickets Here! ----- https://linktr.ee/steveioe
Join the waitlist for Dr. Socko hospital grip socks: https://drsocko.com/
Looking for Blue MuFKR Hoodies? https://mufkr.com/
Find me on
TikTok: https://www.tiktok.com/@steveioe
Instagram: https://www.instagram.com/steveioe
Twitter: https://twitter.com/steveioe
Facebook: https://www.facebook.com/steveioe
P.O. Box:
532308
Los Angeles CA 90053

What goes into providing anesthesia for cardiac surgery where a patient's heart is completely arrested? In this video, I take you into the operating room during a surgery and talk with Dr. Benji Salter, program director for Mt. Sinai Hospital's cardiothoracic anesthesiology fellowship program.
While no patient information is shown in this video, the patient did provide written consent for filming to occur during surgery. Permission was also obtained from Mount Sinai Hospital's Department of Anesthesiology as well as the hospital's Press Office.
Chapters
0:00 Start
0:44 Surgery background
1:40 Case preparation
2:45 Anesthesia equipment
6:21 Echocardiography
7:16 Preparing for bypass
8:34 Stopping the heart
9:06 Fellowship
10:46 Why cardiac anesthesia?
11:52 Coming off of bypass
13:06 Post-op recovery
The information in this video is not intended nor implied to be a substitute for professional medical advice, diagnosis or treatment. All content, including text, graphics, images, and information, contained in this video is for general information purposes only and does not replace a consultation with your own doctor/health professional.
#Anesthesiology #Residency #MedicalSchool

Michigan Medicine’s Cardiac Surgery Simplified series highlights a multitude of surgical procedures in order to educate patients, healthcare providers, and trainees interested in learning about cardiac surgery performed at the Frankel Cardiovascular Center.
Like and subscribe to our channel to learn more about our pioneering procedures including minimally invasive valve surgery and safer methods to repair aortic aneurysms and dissections.
To learn more about cardiac surgery at Michigan Medicine, visit: https://medicine.umich.edu/dept/cardiac-surgery
To learn more about Frankel Cardiovascular Center, visit: https://www.umcvc.org/
To watch the full playlist, visit: https://www.youtube.com/playli....st?list=PLNxqP-XbH8B
-------------------------------------------------------
Subscribe to Michigan Medicine’s YouTube channel for upcoming videos and future live streams featuring our experts answering your questions.
-------------------------------------------------------
Follow Michigan Medicine on Social:
Twitter: https://twitter.com/umichmedicine
Instagram: https://www.instagram.com/umichmedicine/
Facebook: https://www.facebook.com/MichiganMedi...
Follow the U-M Frankel Cardiovascular Center on Social:
Twitter: https://twitter.com/umichcvc
Facebook: https://www.facebook.com/Universityof...
#MichiganMedicine #MedEd #CardiacSurgery #UniversityOfMichiganHealth #FrankelCardiovascularCenter #Cardiology

Cardiac anesthesiology is a subspecialty of anesthesiology that entails caring for patients undergoing major heart surgeries, including those that require cardiopulmonary bypass. I made this video to show a cardiac anesthesiologist's typical setup for surgery.
0:00 Start
0:28 IV pole #1
1:18 Perfusionist equipment
1:47 Anesthesia machine
3:01 Medications
3:36 Pacemaker
4:10 Echocardiography
4:34 IV pole #2
4:55 Arterial line
5:25 Defibrillators
5:40 OR table
---------
Find Max Feinstein, MD online:
Instagram: @MaxMFeinstein
Twitter: @MaxMFeinstein
Website: http://www.MaxFeinsteinMD.com
---------
The information in this video is not intended nor implied to be a substitute for professional medical advice, diagnosis or treatment. All content, including text, graphics, images, and information, contained in this video is for general information purposes only and does not replace a consultation with your own doctor/health professional.
---------
Music
Subtle Swagger by Ron Gelinas Chillout Lounge | https://soundcloud.com/atmospheric-music-portal
Music promoted by https://www.free-stock-music.com
Creative Commons Attribution 3.0 Unported License
https://creativecommons.org/li....censes/by/3.0/deed.e
---------
#Anesthesiology #Residency #MedicalSchool

The CSICU rounds are an opportunity for residents to come together with attendings and review all the patients in the ICU.
Cedars-Sinai is committed to educating exceptional cardiothoracic surgeons through outstanding personal mentorship, operative training and research leadership. Residents of the Thoracic Surgery—Integrated Residency at Cedars-Sinai will be part of an incredibly rich, academic environment—each year our research and thought leadership features in hundreds of publications in journals including Nature, New England Journal of Medicine, JAMA, Lancet and leading specialty journals.
Learn more about the Cedars-Sinai Thoracic Surgery—Integrated Residency: https://ceda.rs/3UDrZFL
Connect with us:
https://twitter.com/CedarsSinai
https://www.facebook.com/CedarsSinai
https://www.instagram.com/CedarsSinai
Cedars-Sinai is a leader in providing high-quality healthcare encompassing primary care, specialized medicine and research. Since 1902, Cedars-Sinai has evolved to meet the needs of one of the most diverse regions in the nation, setting standards in quality and innovative patient care, research, teaching and community service. Today, Cedars- Sinai is known for its national leadership in transforming healthcare for the benefit of patients. Cedars-Sinai impacts the future of healthcare by developing new approaches to treatment and educating tomorrow’s health professionals. Additionally, Cedars-Sinai demonstrates a commitment to the community through programs that improve the health of its most vulnerable residents.

Ellis demonstrates how to clean a reusable inner cannula, care for a tracheostomy site, and suction a tracheostomy.
Our Critical Nursing Skills video tutorial series is taught by Ellis Parker MSN, RN-BC, CNE, CHS and intended to help RN and PN nursing students study for your nursing school exams, including the ATI, HESI and NCLEX.
#ClinicalSkills #NCLEX #tracheostomy #patientcare #ATI #Kaplan #LVN #PN #RN #nurseeducator #nurse #nursingstudent #murse #clinicals #clinicalnursingskills
00:00 What to expect Tracheostomy Care and Suctioning
0:33 Explaining the process Tracheostomy Care and Suctioning
1:10 Positioning patient for a Tracheostomy Care and Suctioning
1:33 Opening tray
1:46 Pouring saline
1:58 Removing inner cannula
2:14 Removing clean gloves
2:25 Donning sterile gloves
3:16 Showing tray contents
3:53 Removing previous dressing
4:06 Pouring saline
4:27 Cleaning stoma
5:10 Cleaning faceplate
5:20 Drying site
5:30 Cleaning inner cannula
6:00 Drying inner cannula
6:20 Reinserting inner cannula
6:40 Placing new gauze
7:00 Replacing ties
8:00 Replacing oxygen
8:13 Preparing for suction
8:58 Checking suction
9:30 Opening saline
9:42 Opening kit
9:58 Donning sterile gloves
11:04 Setting up saline container
11:20 Pouring saline
11:52 Connecting catheter to suction
12:46 Inserting catheter
13:10 Removing catheter
13:24 Rinsing catheter
13:40 Reoxyginating
14:05 Reinserting catheter
14:17 Removing catheter
14:29 Rinsing catheter
14:44 Reoxyginating
14:55 Cleaning up
15:09 Chatting about sterility
17:00 Checking a tie
🚨 Reminder: shipping deadlines are looming 👀
🎁 Regular Shipping: Order by Friday, December 15
🚀 Expedited Shipping: Order by Monday, December 18
🔍 Still searching for last-minute gifts? Consider a Level Up RN Gift Card! 💌 It’s not only a thoughtful present but also the perfect way to share treasures like Pharmacology Flashcards OR digital treasures like Flashables Digital Nursing Flashcards & the Level Up RN membership. Give the gift of knowledge this holiday season! 🧠⚡️💖 bit.ly/LevelUpRNGC
🚪 Access our Cram Courses, Quizzes and Videos all in one ad free space with Level Up RN Membership https://bit.ly/LevelUpRNMembership
Want more ways to MASTER Clinical Skills? Check out our flashcards & videos!
👇👇👇👇👇👇👇👇👇👇
👉 https://bit.ly/clinicalnursingskills 👈
☝️👆☝️👆☝️👆☝️👆☝️👆
This is your one-stop-shop for materials to help you LEARN & REVIEW so you can PASS Nursing School.
🤔🤔🤔 DO YOU WANT TO PASS your classes, proctored exams and the NCLEX? 🤔🤔🤔 Our resources are the best you can buy. They are built with a single goal: help you pass with no fluff. Everything you need, and nothing you don’t. Don’t take our word for it, though! Check out our hundreds of ⭐️⭐️⭐️⭐️⭐️ reviews from nurses who passed their exams and the NCLEX with Level Up RN.
🗂️ Our Ultimate Nursing School Survival kit is your number 1 resource to get through nursing school and to pass the NCLEX. Whether you're just starting school or you’re already prepping for the NCLEX, this bundle of flashcards is the best you can buy. It covers all the information you need to know to pass all your exams and it has FREE shipping!
➡️ https://bit.ly/TUNSSK ⬅️
L👀king for EVEN MORE resources to survive Nursing School? Make your Nursing School experience your own! Life’s difficult enough—learning shouldn’t be.
🪅 Games https://nursesquad.com
💻 Digital resources https://bit.ly/NursingStudyCourses
📅 Organizational tools https://bit.ly/OrganizingSchool
✨Want perks? Join our channel!
https://youtube.com/leveluprn/join
🏷 Head to https://leveluprn.com/specials for all our latest deals!🥳️
📧 LOOKING FOR FREE RESOURCES TO HELP WITH YOUR EXAMS? Get exclusive tips, latest video releases and more delivered to your email!
➡️ https://leveluprn.com/signup ⬅️
⚕ 👩 LEVEL UP NURSE SQUAD 👩⚕️
All of the nurses at Level Up RN are here to help! Cathy Parkes started helping her fellow classmates back when she was in nursing school, tutoring so they could pass their exams and graduate. After she got her BSN and started working as an RN at Scripps Encinitas Hospital, she started this YouTube channel to help nursing students around the world. Since then she has built a team of top-notch dedicated nurses and nurse educators who are focused on improving nursing education and supporting career advancement for nurses everywhere. With flashcards, videos, courses, organizational tools and more, we are singularly focused on helping students and nurses Level Up on their exams and nursing careers.

Ellis demonstrates how to perform a sterile wound dressing change. It would be appropriate to perform hand hygiene between glove changes.
Our Critical Nursing Skills video tutorial series is taught by Ellis Parker MSN, RN-BC, CNE, CHS and intended to help RN and PN nursing students study for your nursing school exams, including the ATI, HESI and NCLEX.
#NCLEX #ClinicalSkills #woundcare #HESI #Kaplan #ATI #NursingSchool #NursingStudent #Nurse #RN #PN #Education #LVN #LPN #nurseeducator
00:00 What to expect
00:51 Prepping for wound dressing change
1:15 Removing the old wound dressing
1:40 Assessing a wound
2:05 Setting up sterile field
2:49 Sterile gloving
4:02 Preparing equipment for wound dressing change
5:09 Cleaning a wound
6:13 Drying a wound
6:28 Packing a wound
7:19 Covering a wound
7:47 Labeling a wound dressing
🚨 Reminder: shipping deadlines are looming 👀
🎁 Regular Shipping: Order by Friday, December 15
🚀 Expedited Shipping: Order by Monday, December 18
🔍 Still searching for last-minute gifts? Consider a Level Up RN Gift Card! 💌 It’s not only a thoughtful present but also the perfect way to share treasures like Pharmacology Flashcards OR digital treasures like Flashables Digital Nursing Flashcards & the Level Up RN membership. Give the gift of knowledge this holiday season! 🧠⚡️💖 bit.ly/LevelUpRNGC
🚪 Access our Cram Courses, Quizzes and Videos all in one ad free space with Level Up RN Membership https://bit.ly/LevelUpRNMembership
Want more ways to MASTER Clinical Skills? Check out our flashcards & videos!
👇👇👇👇👇👇👇👇👇👇
👉 https://bit.ly/clinicalnursingskills 👈
☝️👆☝️👆☝️👆☝️👆☝️👆
This is your one-stop-shop for materials to help you LEARN & REVIEW so you can PASS Nursing School.
🤔🤔🤔 DO YOU WANT TO PASS your classes, proctored exams and the NCLEX? 🤔🤔🤔 Our resources are the best you can buy. They are built with a single goal: help you pass with no fluff. Everything you need, and nothing you don’t. Don’t take our word for it, though! Check out our hundreds of ⭐️⭐️⭐️⭐️⭐️ reviews from nurses who passed their exams and the NCLEX with Level Up RN.
🗂️ Our Ultimate Nursing School Survival kit is your number 1 resource to get through nursing school and to pass the NCLEX. Whether you're just starting school or you’re already prepping for the NCLEX, this bundle of flashcards is the best you can buy. It covers all the information you need to know to pass all your exams and it has FREE shipping!
➡️ https://bit.ly/TUNSSK ⬅️
L👀king for EVEN MORE resources to survive Nursing School? Make your Nursing School experience your own! Life’s difficult enough—learning shouldn’t be.
🪅 Games https://nursesquad.com
💻 Digital resources https://bit.ly/NursingStudyCourses
📅 Organizational tools https://bit.ly/OrganizingSchool
✨Want perks? Join our channel!
https://youtube.com/leveluprn/join
🏷 Head to https://leveluprn.com/specials for all our latest deals!🥳️
📧 LOOKING FOR FREE RESOURCES TO HELP WITH YOUR EXAMS? Get exclusive tips, latest video releases and more delivered to your email!
➡️ https://leveluprn.com/signup ⬅️
⚕ 👩 LEVEL UP NURSE SQUAD 👩⚕️
All of the nurses at Level Up RN are here to help! Cathy Parkes started helping her fellow classmates back when she was in nursing school, tutoring so they could pass their exams and graduate. After she got her BSN and started working as an RN at Scripps Encinitas Hospital, she started this YouTube channel to help nursing students around the world. Since then she has built a team of top-notch dedicated nurses and nurse educators who are focused on improving nursing education and supporting career advancement for nurses everywhere. With flashcards, videos, courses, organizational tools and more, we are singularly focused on helping students and nurses Level Up on their exams and nursing careers.

Ellis will be demonstrating how to complete an occupied bed change. It would be appropriate to wear gloves during this skill to avoid contact with bodily fluids.
Our Critical Nursing Skills video tutorial series is taught by Ellis Parker MSN, RN-BC, CNE, CHS and intended to help RN and PN nursing students study for your nursing school exams, including the ATI, HESI and NCLEX.
#NCLEX #ClinicalSkills #HESI #Kaplan #ATI #NursingSchool #NursingStudent #Nurse #RN #PN #Education #LVN #LPN #bedmaking #nurseeducator
00:00 What to expect
00:53 Initial patient position
1:50 Tucking soiled linens
2:20 Placing initial clean linen
3:30 Rolling patient
3:40 Removing soiled linen
4:05 Completing bottom layer
4:33 Changing pillow case
4:50 Top sheet and blanket
7:23 Mitered corner
🚨 Reminder: shipping deadlines are looming 👀
🎁 Regular Shipping: Order by Friday, December 15
🚀 Expedited Shipping: Order by Monday, December 18
🔍 Still searching for last-minute gifts? Consider a Level Up RN Gift Card! 💌 It’s not only a thoughtful present but also the perfect way to share treasures like Pharmacology Flashcards OR digital treasures like Flashables Digital Nursing Flashcards & the Level Up RN membership. Give the gift of knowledge this holiday season! 🧠⚡️💖 bit.ly/LevelUpRNGC
🚪 Access our Cram Courses, Quizzes and Videos all in one ad free space with Level Up RN Membership https://bit.ly/LevelUpRNMembership
Want more ways to MASTER Clinical Skills? Check out our flashcards & videos!
👇👇👇👇👇👇👇👇👇👇
👉 https://bit.ly/clinicalnursingskills 👈
☝️👆☝️👆☝️👆☝️👆☝️👆
This is your one-stop-shop for materials to help you LEARN & REVIEW so you can PASS Nursing School.
🤔🤔🤔 DO YOU WANT TO PASS your classes, proctored exams and the NCLEX? 🤔🤔🤔 Our resources are the best you can buy. They are built with a single goal: help you pass with no fluff. Everything you need, and nothing you don’t. Don’t take our word for it, though! Check out our hundreds of ⭐️⭐️⭐️⭐️⭐️ reviews from nurses who passed their exams and the NCLEX with Level Up RN.
🗂️ Our Ultimate Nursing School Survival kit is your number 1 resource to get through nursing school and to pass the NCLEX. Whether you're just starting school or you’re already prepping for the NCLEX, this bundle of flashcards is the best you can buy. It covers all the information you need to know to pass all your exams and it has FREE shipping!
➡️ https://bit.ly/TUNSSK ⬅️
L👀king for EVEN MORE resources to survive Nursing School? Make your Nursing School experience your own! Life’s difficult enough—learning shouldn’t be.
🪅 Games https://nursesquad.com
💻 Digital resources https://bit.ly/NursingStudyCourses
📅 Organizational tools https://bit.ly/OrganizingSchool
✨Want perks? Join our channel!
https://youtube.com/leveluprn/join
🏷 Head to https://leveluprn.com/specials for all our latest deals!🥳️
📧 LOOKING FOR FREE RESOURCES TO HELP WITH YOUR EXAMS? Get exclusive tips, latest video releases and more delivered to your email!
➡️ https://leveluprn.com/signup ⬅️
⚕ 👩 LEVEL UP NURSE SQUAD 👩⚕️
All of the nurses at Level Up RN are here to help! Cathy Parkes started helping her fellow classmates back when she was in nursing school, tutoring so they could pass their exams and graduate. After she got her BSN and started working as an RN at Scripps Encinitas Hospital, she started this YouTube channel to help nursing students around the world. Since then she has built a team of top-notch dedicated nurses and nurse educators who are focused on improving nursing education and supporting career advancement for nurses everywhere. With flashcards, videos, courses, organizational tools and more, we are singularly focused on helping students and nurses Level Up on their exams and nursing careers.

Vital signs help us assess patients in the nursing profession, and there are six common vital signs that we assess as nurses:
1. Heart Rate (Pulse)
2. Respiration Rate
3. Temperature
4. Blood Pressure
5. Pain Rating
6. Oxygen Saturation
This video will demonstrate how to check vital signs (live) on a patient, along with normal rates for each assessment. I also give you a few tips for taking vital signs as a nurse, CNA, or other healthcare profession.
🟣ABG eBook: https://registerednursern.creator-spring.com/
🟣ABG physical book: https://amzn.to/3EsF0Mc (affiliate link)
More nursing skills: https://www.youtube.com/watch?v=G5-Rp-6FMCQ&list=PLQrdx7rRsKfUhd_qQYEbp0Eab3uUKhgKb
Website: https://www.registerednursern.com/
More Videos: https://www.youtube.com/watch?v=R2XMro13dD0&list=UUPyMN8DzkFl2__xnTEiGZ1w
Nursing Gear: https://teespring.com/stores/registerednursern
Instagram: https://www.instagram.com/registerednursern_com/
Facebook: https://www.facebook.com/RegisteredNurseRNs
Twitter: https://twitter.com/NursesRN
Popular Playlists:
NCLEX Reviews: https://www.youtube.com/playli....st?list=PLQrdx7rRsKf
Fluid & Electrolytes: https://www.youtube.com/playli....st?list=PLQrdx7rRsKf
Nursing Skills: https://www.youtube.com/playli....st?list=PLQrdx7rRsKf

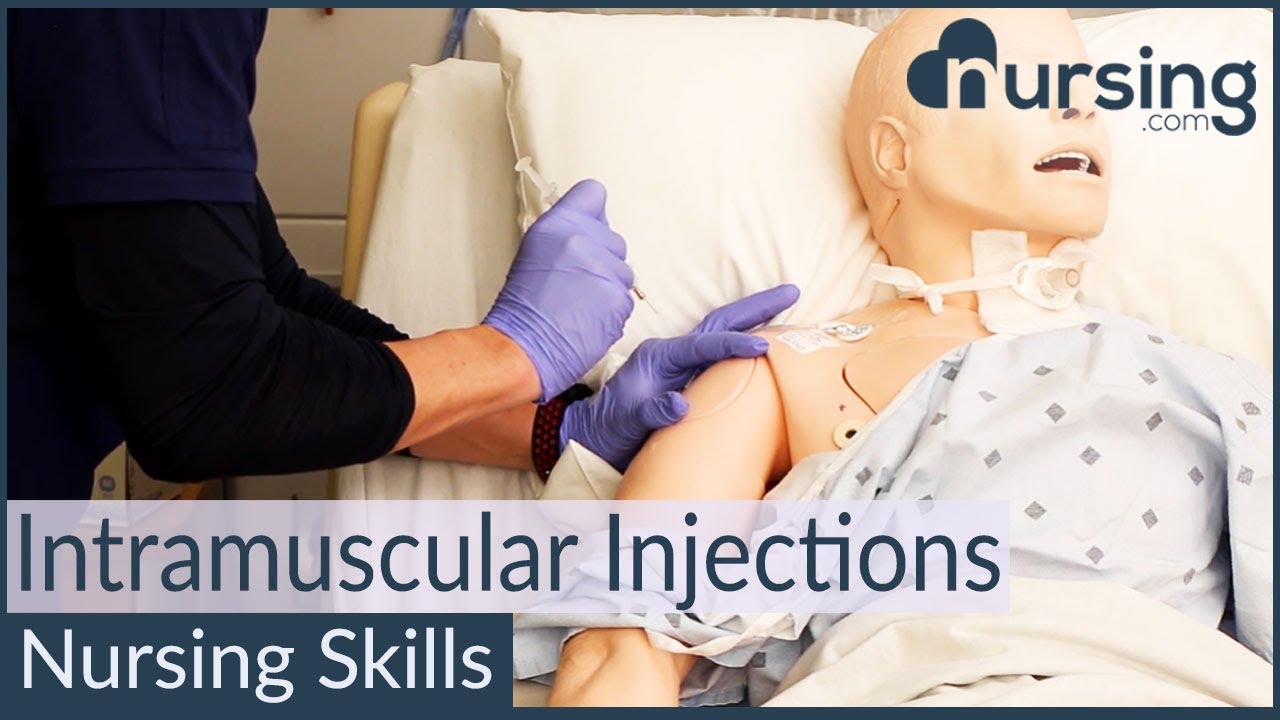
WATCH MORE NURSING SKILLS HERE: https://nursing.com/course/nursing-skills/?utm_source=youtube&utm_medium=social
In our Nursing Skills course, we show you the most common and most important skills you will use as a nurse! We included everything from bed baths, to inserting a foley, to advanced skills like chest tube management.
Welcome to the NURSING Family, we call it the most supportive nursing cohort on the planet.
At NURSING.com, we want to help you remove the stress and overwhelm of nursing school so that you can focus on becoming an amazing nurse.
Check out our freebies and learn more at: (http://www.nursing.com)
Visit us at http://www.nursing.com/medical....-information-disclai for disclaimer information.
NCLEX®, NCLEX-RN® are registered trademarks of the National Council of State Boards of Nursing, INC. and hold no affiliation with NURSING.
FREE Nursing School Cheat Sheets at: http://www.NURSING.com
Get the full lesson on IM Injections here:
https://nursing.com/lesson/ski....lls-06-01-pill-crush
Check out our new Nurse Care Plan Lessons here:
https://bit.ly/3BPRfPL
Get Access to Thousands of Lessons here:
https://nursing.com/courses/
Welcome to the NURSING Family, we call it the most supportive nursing cohort on the planet.
At NURSING.com, we want to help you remove the stress and overwhelm of nursing school so that you can focus on becoming an amazing nurse.
Check out our freebies and learn more at: (http://www.nursing.com)
Intramuscular Injection Techniques (Nursing Skills)
In this video, we’re going to look at proper administration techniques for intramuscular medication administration. Of course, always follow your 5 rights and calculate the correct volume for administration. We love you guys! Go out and be your best selves today! And, as always, happy nursing!
Bookmarks:
0.05 Introduction to Intramuscular injections
0.16 site and needle selection
0.35 site sterilization
0.43 Z track method
0.58 needle insertion
1.10 medication injection
1.14 needle removal
1.25 bandaging and needle disposal
1.30 documentation and patient monitoring
1.35 Outro
Visit us at https://nursing.com/medical-disclaimer/ for disclaimer information.
NCLEX®, NCLEX-RN® are registered trademarks of the National Council of State Boards of Nursing, INC. and hold no affiliation with NURSING.com.

http://www.utexas.edu
Nursing students practice their skills on mannequins and each other in the Nursing Skills Lab.

Health Assessment: Musculoskeletal System- Nursing Skills
FREE Nursing School Cheat Sheets at: http://www.NURSING.com
Get the full lesson on musculoskeletal assessment here:
https://nursing.com/lesson/02-11-musculoskeletal/
Welcome to the NURSING Family, we call it the most supportive nursing cohort on the planet.
At NURSING.com, we want to help you remove the stress and overwhelm of nursing school so that you can focus on becoming an amazing nurse.
Check out our freebies and learn more at: (http://www.nursing.com)
Health Assessment: Musculoskeletal System- Nursing Skills:
In this video we’re going to review a Musculoskeletal Assessment. The Musculoskeletal system involves the muscles, bones, and joints. This means we must assess structure AND function! If the patient cannot stand, assessments should be performed in the bed to the best of your ability. If they cannot perform Active Range of Motion (ROM), use Passive movements to determine ROM.
We love you guys! Go out and be your best selves today! And, as always, happy nursing!
Bookmarks:
0.05 Introduction
0:34 Spine assessment
1:02 Range of motion
1:39 Extremity assessment
1:52 Shoulder range of motion
2:10 Elbow & wrist range of motion
2:25 Hand range of motion
2:34 Upper extremity strength
2:54 Lower extremity range of motion
3:02 Hips range of motion
3:20 Knees range of motion
3:30 Ankles range of motion
3:38 Toes range of motion
3:42 Lower extremity strength
4:05 Outro
Visit us at https://nursing.com/medical-disclaimer/ for disclaimer information.
NCLEX®, NCLEX-RN® are registered trademarks of the National Council of State Boards of Nursing, INC. and hold no affiliation with NURSING.com.

If you’ve lost a significant amount of weight, either after pregnancy or through exercise and dietary changes, excess skin and weakened abdominal muscles can leave you self-conscious about your appearance. In this video, Dr. Catherine Hannan and Dr. Lauren Patrick, two of our Board-Certified Plastic Surgeons, are performing a Tummy Tuck (Abdominoplasty) surgery. Tummy Tuck surgery gets rid of the excess skin, as well as tightens your abdominal muscles, resulting in a flatter and smoother abdomen. The results of the surgery are permanent except in cases of large weight gain or pregnancy after surgery.
We are so excited to have taken a part in our patient's body transformation journey!
Before & After Gallery:
https://www.westendplasticsurg....ery.com/surgical/bod
To learn more, visit our website or call (202) 785-4187
http://www.westendplasticsurgery.com
~~~~~~~~~~~~~~~~~~~
Social Media:
✨ Instagram: http://www.instagram.com/westendplasticsurgery
✨ Facebook: http://www.facebook.com/westendplasticsurgery
✨ Twitter: http://www.twitter.com/weplasticsurg
✨ Blog: https://www.westendplasticsurgery.com/blog
✨ Business Inquiries: info@westendplasticsurgery.com
~~~~~~~~~~~~~~~~~~~
#TummyTuck #Abdominoplasty
Tummy tuck Sydney Dr Barnouti. Call us on 02-9561 0222 or 1300 002 006
Broadway, Chatswood, Burwood NSW Australia
email:drbarnouti@australiaplasticsurgery.com.au
https://www.plasticsurgery-syd....ney.com.au/abdominop
What is a tummy tuck?
A tummy tuck operation is also known as abdominoplasty. It involves removing excess skin and fat from the stomach area, mainly the lower part of the tummy through surgical procedure. A tummy tuck operation is intended to leave the patient with a flatter tummy and to remove any signs of an 'apron' stomach or an overhang which is sometimes visible above underwear. The skin on this area tends to be stretched and of poor quality. A tummy tuck operation will usually focus on the lower part of the stomach, below the belly button and may require the belly button to be repositioned in some cases. The procedure is often carried out on women or men who have suffered from stretched skin in the stomach area after pregnancy, giving birth, excess fat deposition or weight loss.
What happens during a tummy tuck?
During a tummy tuck procedure the aim of the surgeon is to cut away fat and excess skin. To do this Dr Barnouti will make in incision on the lowest part of the stomach, where a fold will be visible above the pubic bone. He will take out as much excess fat as can be removed and will then cut the skin to fit back over the place where the fat has been removed from. It is important to have realistic expectations of a tummy tuck. Taking too much fat and skin away can result in folds at each end of the resulting scar which are sometimes referred to as "dog ears". Dr Barnouti will make sure you will not have this problem.
Who should have a tummy tuck?
Tummy tucks are recommended for either men or women who have an excess of fat and skin around their abdomen which cannot be removed by weight loss, exercise or liposuction. Tummy tuck operations in women are usually reserved for those who are not likely to have children as it is inadvisable to get pregnant again after having skin removed, this can cause the wound to stretch and scar.
The cost of a tummy tuck in Sydney Australia
The total cost is $7,900 if the patient's health fund cover the hospital's fees. In case the health fund does not cover the hospital's fee, the total cost will be around $12,000 inclusive of the Surgeon, assistant surgeon, Anaesthetist, hospital, operating theatre and follow ups visit.
Payment plans are alos available from Dr Barnouti's office in Chatswood, Burwood or Broadway.
A tummy tuck is a cosmetic procedure that removes excess skin and fatty tissue in order to give a flatter appearance to the stomach. Tummy tucks, also known as abdominoplasties, are ideal for patients who are not excessively overweight but suffer from an overhang of skin around the abdomen.
Performed under general anaesthetic, tummy tucks involve a horizontal incision being made just above the pubic area between the hip bones. Skin and fatty tissue is separated from the muscle and the area is tightened, with the excess skin and fatty tissues then being pulled downwards and removed.
Following your tummy tuck, there will be a scar present across the lower abdomen, but this will gradually fade. You may experience moderate tissue swelling for several months, but this will disappear with time. There may also be a sensation reduction just above the pubic area.
Once your tummy tuck recovery is complete however, you'll benefit from a more attractive figure and the ability to wear a wider selection of clothes.






