Top videos

Routine pelvic exams are important for good reproductive health. A woman should have her first GYN exam when she first thinks about becoming sexually active, when she becomes sexually active or when she turns 18.
At the gynecologist, you will have a short general physical exam, including a breast exam. You will wear a hospital gown and nothing else. For the actual pelvic examination, you will lie down on an examination table with your feet resting in elevated “stirrups” (props that support your legs in the air). Stirrups might look a little scary, but they are there to keep you comfortable. Your legs will be spread apart, with your knees falling to each side so that your vagina is exposed. You may feel uncomfortable, but relax and realize that everyone goes through this.
External Exam
The practitioner will visually examine your vulva for discoloration, irritation, swelling and other abnormalities, and will gently feel for glands.
Internal Exam
There are two parts to the internal exam. The first involves a speculum, a metal or plastic instrument that the practitioner inserts into the vagina. The speculum is shaped like a duck’s bill, and once it is inserted into the vaginal canal, it is gently widened to spread the interior vaginal walls (this is not painful). As the vaginal walls are spread, the practitioner is able to see the walls of the vagina itself, and up the vaginal canal to the cervix. When viewing the vaginal canal and the cervix, the practitioner can look for discoloration, abnormal discharge, lesions, growths and signs of infection. It is possible for you to look at your own cervix during this process by propping yourself up on your elbows and using a mirror. Some practitioners ask if you would like to do this, but feel free to ask to if she doesn’t mention it first.
Pap Smear
Next the practitioner will take a pap smear. She/he uses a long-stemmed cotton swab to collect a sample of cells in the cervix. Some women feel a slight cramping sensation when their cervix is touched. The collected cells are smeared onto a slide and sent to a lab for testing and examination. The pap smear is extremely important for spotting abnormalities in the cervix which may indicate infection or disease.
STD Testing
If you are sexually active, the practitioner will test for STDs. The gynecologist will swab the inside of the cervix with a long cotton swab. The speculum is then taken out of the vagina. The samples are sent to a laboratory for various STD testing. The tests will probably take a couple days. Ask when your results will be available so you can call. If you want to be tested for HIV, syphilis, genital herpes or hepatitis you need to have blood taken. They can do that as well, but you will need to ask since it is not usually routine.
Manual Exam
The second part of the pelvic exam is called the manual or bi-manual exam. The practitioner will insert one or two fingers into your vagina and press with her/his other hand on the outside of your lower abdomen. They will use a lubricant on their fingers so it is more comfortable. The person can then feel the uterus, fallopian tubes and ovaries, and check for any swelling or tenderness. Once the doctor is finished checking your uterus and ovaries, the exam is complete. The entire pelvic exam (the parts involving your vagina, cervix, uterus, and ovaries) takes 3 to 5 minutes to complete.

ectal exam is an internal examination of the rectum such as by a physician or other healthcare professional.
The digital rectal examination (DRE, Latin palpatio per anum or PPA) is a relatively simple procedure. The patient is placed in a position where the anus is accessible and relaxed (lying on the side, squatting on the examination table, bent over the examination table, etc). The physician inserts a gloved and lubricated finger into the rectum through the anus and palpates the insides.
The DRE is inadequate as a screening tool for colorectal cancer because it examines less than 10% of the colorectal mucosa; colonoscopy is preferred. However, it's an important part of a general examination, as many tumors or other diseases are made manifest in the distal part of the rectum.
This examination may be used: * for the diagnosis of rectal tumors and other forms of cancer; * in males, for the diagnosis of prostatic disorders, notably tumors and benign prostatic hyperplasia; * for the diagnosis of appendicitis or other examples of an acute abdomen (i.e. acute abdominal symptoms indicating a serious underlying disease); * for the estimation of the tonicity of the anal sphincter, which may be useful in case of fecal incontinence or neurologic diseases, including traumatic spinal cord injuries; * in females, for gynecological palpations of internal organs * for examination of the hardness and color of the feces (ie. in cases of constipation, and fecal impaction); * prior to a colonoscopy or proctoscopy. * to evaluate haemorrhoids
The DRE is frequently combined with an FOBT (fecal occult blood test), which may be useful for diagnosing the etiology of an anemia and/or confirming a gastrointestinal bleed.
Sometimes proctoscopy may also be part of a rectal examination.
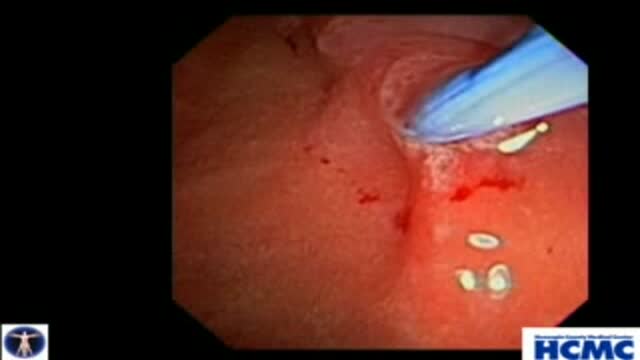
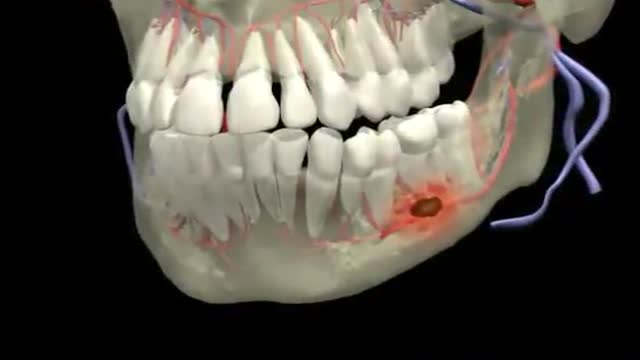
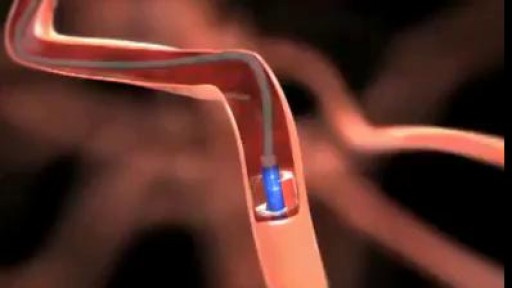
Biliary and Pancreatic Sphincterotomies for Sphincter of Oddi Dysfunction
This 43 year old woman has severe recurrent RUQ pain post cholecystectomy. Liver and pancreatic chemistries and duct size are normal, but pancreatic manometry is abnormal. The plan is to perform dual biliary and pancreatic sphincterotomy. The pancreatic duct is cannulated with a 3.9 French tip tr...iple lumen papillotome loaded with a 0.025 inch Jagwire. Contrast is injected to outline the course of the duct. The wire is passed to the tail. Notice the knuckling of the wire into the tail. This provides a safety loop, but is only safe in a small duct with use of a smaller caliber wire. Then with the wire securely in PD, papillotome is used to cannulate the bile duct. Placement of the wire in PD guarantees access for pancreatic stent placement, which is mandatory in these patients to reduce risk, it also facilitates difficult biliary cannulation. Here is the fluoroscopic view as the papillotome is passed deep into bile duct. This shows wires in the CBD and PD. Now a biliary sphincterotomy is performed, with the pancreatic guidewire in place beside the papillotome. The scope is pushed into a longer position to orient up the middle of the papilla. The sphincterotomy is done in very careful stepwise fashion to avoid perforation. Now the biliary wire is removed and the papillotome passed over the pancreatic wire for pancreatic sphincterotomy. The incision is aimed back up towards the biliary sphincterotomy to ensure the septum only is cut. Note the large pancreatic orifice. Last, a 4 French 9cm unflanged soft material pancreatic stent is placed. We always use single pigtail design to avoid inward migration of the stent. The long unflanged design allows spontaneous passage within a few weeks.

New Minimally Invasive Procedure with No Pain or Downtime… From Dr. Michael Goodman, Caring For Women Wellness Center Laser Vaginal Tightening for Improved Sexual Pleasure and Relief from Minimal Urinary Incontinence Laser Vaginal Therapy for reversing Vaginal Atrophy (Good also for Breast Cancer Survivors with Vaginal Atrophy)

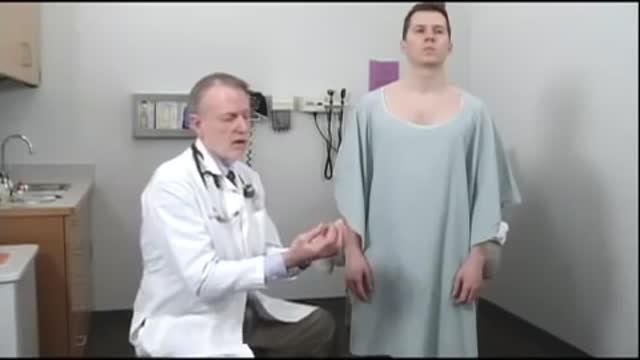
Introduction to the Brachial Plexus Examination, 4 of 5 videos demonstrating the physical exam for evaluation of Brachial Plexus conditions.
Brachial plexus injury - Care at Mayo Clinic:
https://www.mayoclinic.org/dis....eases-conditions/bra
Watch all the videos in this series on this playlist:
https://www.youtube.com/playli....st?list=PLSWR1ylG_6J

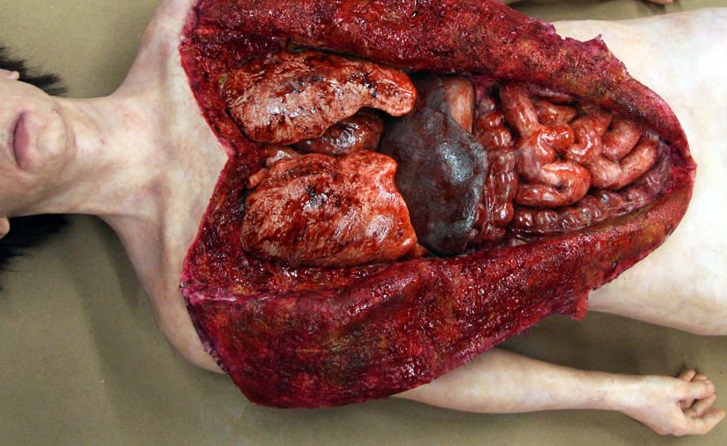
Dr. Celia Divino, Chief, Division of General Surgery at The Mount Sinai Hospital, performs a laparoscopic appendectomy. Visit the Division of General Surgery at http://bit.ly/18z944M. Click here to learn more about Dr. Celia Divino http://bit.ly/12RF0ee