Top videos
Face transplant allows this man to live a normal life. Hats off to all the surgeons involved!
How to prepare for Gynecomastia Surgery?|Male Breast Reduction Surgery |Dr Rajat Gupta RG Aesthetics
Gynecomastia is the most common breast problem afflicting men. It can be the source of
significant social embarrassment, which is the reason some seek medical advice. The main reason why people undergo Gynecomastia Surgery is that they have body image issues and social inhibitions, as a result, they tend to avoid activities wherein they have to showcase their body. Gynecomastia can be socially devastating, this can hamper one's self-esteem and confidence.
Gynecomastia surgery / Male Breast Reduction Surgery
Gynecomastia surgery is also known as male breast reduction, is an excellent solution for those men who struggle with the condition of having overdeveloped breasts. The main aim of Gynecomastia surgery is to provide the patients with the desired result of the masculine chest along with no scars / without any visible scar. So it is very important to discuss with your doctor about gynecomastia surgery procedure as well as to ensure that there won't be any visible scarring.
How to prepare for Gynecomastia Surgery/ Male Breast Reduction Surgery?
Dr Rajat Gupta performs the surgery in such a way that there is no visible scarring. He uses a technique wherein a very small incision of 3-4mm is made on the side of the chest. Later he uses a device called as Microaire which breaks down the glands inside and removes the glands from the same incision. Later Dr Rajat Gupta uses a tool called Vaser which heats up the skin and tightens it. It is very important to ensure all of this.
Also, before the surgery, the patient needs to ensure before the surgery that "what will be the recovery procedure ?". The patient needs to prepare himself with answers to all of these. Gynecomastia surgery is a daycare surgery and this surgery has a fast recovery process.
The results are visible immediately. Before going for gynecomastia surgery make sure you try to get all the information related to Gynecomastia surgery, discuss with your doctor regarding the scar-free Gynecomastia treatment and prepare yourself Gynaecomastia surgery. If you are suffering from Gynecomastia do not hesitate to get Gynecomastia surgery.
Be a part of our Gynecomastia community.
✅ Get insights from our patient community
✅ Ask our board-certified plastic surgeons anything
✅ View the before-and-after patients' results
✅ Connect with other patients & ask them about their experience
✅ First of its a kind initiative in INDIA for patient education and interaction
Join our community: https://drrajatgupta.com/community/
Gynecomastia Helpline: +91 95689 99333
_______________________________________
About Dr Rajat Gupta and RG Aesthetics
At RG Aesthetics, India’s best plastic surgeon, Dr Rajat Gupta is at your service! With 10 years of experience, brand-certification, and international recognition, Dr Gupta is the solution to all your contouring needs.
His expertise in liposuction techniques combined with the state-of-the-art technology available at RG Aesthetics ensures we continue providing the most reliable services with incredible, instantaneous results!
Our equipment allows for every kind of liposuction there is – especially the minimal invasive kinds. Dr Gupta reflects RG Aesthetics’ belief of the patient’s comfort always being paramount. Procedures at RG Aesthetics, under Dr Rajat Gupta, minimize trauma and speed up recovery time for the best results!
For more information please visit our website: https://www.drrajatgupta.com/
For more details,
contact us:+91-9251-711-711 or contact@drrajatgupta.com
#gynaecomastia #gynaecomastiasurgery #preparegynaecomastiasurgery #drrajatgupta #rgaesthetics
An ectopic pregnancy results when a fertilized egg implants outside the uterus. Unfortunately, there's no way to transplant an ectopic pregnancy into your uterus, so ending the pregnancy is the only option. About 2 percent of pregnancies are ectopic. Because ectopic pregnancy is potentially dangerous for you, it's important to recognize the early signs and get treatment as soon as possible.
A penile prosthesis is another treatment option for men with erectile dysfunction (ED). These devices are either malleable or inflatable. The simplest type of prosthesis consists of a pair of malleable (bendable) rods surgically implanted within the erection chambers of the penis. With this type of implant the penis is always semi-rigid and merely needs to be lifted or adjusted into the erect position to initiate sex. Today, many men choose a hydraulic, inflatable prosthesis, which allows a man to have an erection whenever he chooses and is much easier to conceal. It is also more natural.
Buy Double X Power medication from rsmenterprises.in is used in erectile dysfunction and premature ejaculation treatment in men. The medication encompasses Buy Sildenafil 100mg and Dapoxetine in 60mg of proportion.
Buy Now : https://tinyurl.com/buy-double-x-power
#rsmenterprises #health #healthcare #doublexpower #sildenafil100mg #dapoxetine60mg #edmedicine #maleedmedicine
HOW BABY GROWS IN THE WOMB DURING PREGNANCY
Order Sildigra Super Power (Sildenafil 100mg + Dapoxetine 60mg) today from a trusted online pharmacy and experience the benefits of this advanced solution for ED and premature ejaculation.
Buy Now : https://tinyurl.com/Buy-Sildigra-Super-Power
#rsmenterprises #health #healthcare #sildigrasuperpower #sildenafil100mg #dapoxetine60mg #genericviagra #maleedmedicine
Back Massage
Terrifying Sinus Infection - Disturbing - Must Watch
Kamagra Oral Jelly is a prescription medication containing sildenafil citrate used to treat erectile dysfunction in men. Buy Kamagra Oral Jelly, a quick-acting, easy-to-use, and highly successful treatment.
Buy Now : https://tinyurl.com/purchase-now-kamagraoraljelly
#rsmenterprises #health #healthcare #menshealth #kamagraoraljelly #sildenafiloraljelly #genericviagraoraljelly
Dimple Creation Surgery | Dimpleplasty | Procedure of Dimple Creation |Dr Rajat Gupta, RG Aesthetics
Dimples creation Surgery/ Dimpleplasty is a type of plastic surgery used to create dimples on the cheeks. Dimples are the indentations that occur when some people smile. They’re most often located on the bottoms of the cheeks. Not everyone is born with this facial trait. In some people, dimples are naturally occurring due to defect in smiling muscle. Dimples are perceived as a sign of beauty.
How dimples are formed?
Dimples are formed because of the defect in the smiling muscle called Zygomaticus Major. A very small part of this muscle is attached to the skin. So whenever a person smiles the skin lying over this defect gets wedged into it, in the connective tissue, creating dimples.
Dimple creation is a simple procedure of fewer than 20 minutes. Before undergoing the surgery the patient consults the doctors and decides the size and location of the dimple they want.
The procedure of Dimple Creation
1.Before the surgery the doctors mark the position of the dimple based on patients on where the patient wants the dimple. The doctor also guides the patient regarding the position of dimples.
2.This surgery is performed under local anaesthesia.
3.Doctors perform this surgery from inside the mouth (inside of the cheek) in order to ensure there are no scars on the face. A small cut of 3-4mm is made inside the cheek area.
4.After making this incision, depending on where you want the dimple, a suture is passed through. This connects your skin to the underlying muscle, creating the dimple. You can see the dimple immediately.
_______________________________________
About Dr Rajat Gupta and RG Aesthetics
At RG Aesthetics, India’s best plastic surgeon, Dr Rajat Gupta is at your service! With 10 years of experience, brand-certification, and international recognition, Dr Gupta is the solution to all your contouring needs.
His expertise in liposuction techniques combined with the state-of-the-art technology available at RG Aesthetics ensures we continue providing the most reliable services with incredible, instantaneous results!
Our equipment allows for every kind of liposuction there is – especially the minimal invasive kinds. Dr Gupta reflects RG Aesthetics’ belief of the patient’s comfort always being paramount. Procedures at RG Aesthetics, under Dr Rajat Gupta, minimize trauma and speed up recovery time for the best results!
For more information please visit our website: https://www.drrajatgupta.com/
For more details,
contact us:+91-9251-711-711 or contact@drrajatgupta.com
#howtocreatedimples #dimplecreationsurgery #dimpleplasty #drrajatgupta #rgaesthetics
Absence seizures involve brief, sudden lapses of consciousness. They're more common in children than adults. Someone having an absence seizure may look like he or she is staring into space for a few seconds. This type of seizure usually doesn't lead to physical injury. Absence seizures usually can be controlled with anti-seizure medications. Some children who have them also develop other seizures. Many children outgrow absence seizures in their teens.
If you are looking for the treatment of premature ejaculation (PE) then there is a highly effective product called poxet 60mg.Millions of men suffer from PE, a frequent sensual dysfunction characterized by a persistent or recurrent inability to delay ejaculation on sensual stimulation.You can buy Poxet 60mg tablets online.The active substance of the product is Dapoxetine, an SSRI (selective serotonin reuptake inhibitor). Dapoxetine delays ejaculation by raising the level of serotonin in the brain, that's how it works. It is not meant to be taken every day like medication. Take as needed, 1 to 3 hours prior to sensual play. No more than a single tablet is to be taken within a 24-hour period. It is worth visiting your doctor prior to taking this product. To find out if this is appropriate and safe for you, your doctor will examine any existing health condition that you may have as well as any other medications that you may be using. Additionally, you should report promptly to your physician in the event of unusual symptoms experienced by you when on Poxet 60mg.Buy Poxet 60mg online at our web store https://www.firstchoicemedss.com/poxet-60mg.html
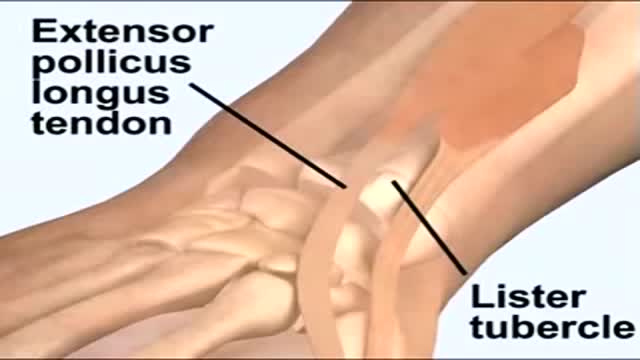
A needle is inserted into a joint for two main indications: aspiration of fluid (arthrocentesis) for diagnosis or for relief of pressure, or injection of medications. In practical terms, most injections into joints consist of a glucocorticoid, a local anesthetic, or a combination of the two. Occasionally saline is injected into the joint to diagnose a joint injury. This topic will review the basic technique of inserting a needle into a joint and the main indications for intraarticular steroid injections. The same techniques apply for injection of the less commonly used hyaluronate viscosupplementation agents into knees, hips, and perhaps shoulders.
Snovitra Super power 80mg is a truly effective blend for the treatment of ED and PE in males.This product is a mixture of Vardenafil and Dapoxetine, which are two active pharmaceutical ingredients within that contain synergistic action on the body to provide dual action therapy for these two diseases. Vardenafil belongs to the drug class known as the PDE5 inhibitors that increase blood flow to the male genital organ and thereby make erection possible for him. Dapoxetine, however, is an SSRI that is active through the serotonin level increase in the brain which leads to delaying the ejaculation.You can buy snovitra super power 80 mg tablets online. The patient can swallow the tablet with a glass of water half an hour before sensual play. The duration of the medication's effects can be as long as 4-6 hours, while sensual activity can be prolonged. But it should be kept in mind that this product is not to be used more than once daily and should be consumed only after consultation with a medical professional. It should not be consumed by persons having severe liver or renal diseases, heart disease, hypotension, or any other of the patient's drugs like nitrates.Buy Snovitra Super Power 80mg online at our web store https://www.firstchoicemedss.c....om/snovitra-super-po
Implant comparison: Coloplast vs AMS for Penile Implants
Michigan Medicine’s Cardiac Surgery Simplified series highlights a multitude of surgical procedures in order to educate patients, healthcare providers, and trainees interested in learning about cardiac surgery performed at the Frankel Cardiovascular Center.
Like and subscribe to our channel to learn more about our pioneering procedures including minimally invasive valve surgery and safer methods to repair aortic aneurysms and dissections.
To learn more about cardiac surgery at Michigan Medicine, visit: https://medicine.umich.edu/dept/cardiac-surgery
To learn more about Frankel Cardiovascular Center, visit: https://www.umcvc.org/
To watch the full playlist, visit: https://www.youtube.com/playli....st?list=PLNxqP-XbH8B
-------------------------------------------------------
Subscribe to Michigan Medicine’s YouTube channel for upcoming videos and future live streams featuring our experts answering your questions.
-------------------------------------------------------
Follow Michigan Medicine on Social:
Twitter: https://twitter.com/umichmedicine
Instagram: https://www.instagram.com/umichmedicine/
Facebook: https://www.facebook.com/MichiganMedi...
Follow the U-M Frankel Cardiovascular Center on Social:
Twitter: https://twitter.com/umichcvc
Facebook: https://www.facebook.com/Universityof...
#MichiganMedicine #MedEd #CardiacSurgery #UniversityOfMichiganHealth #FrankelCardiovascularCenter #Cardiology
Procedures Requiring General Anaesthesia
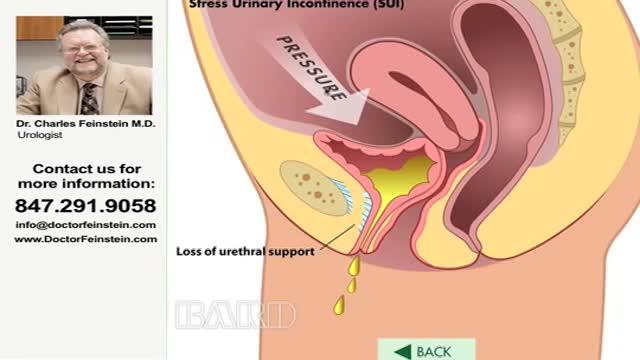
Urinary incontinence — the loss of bladder control — is a common and often embarrassing problem. The severity ranges from occasionally leaking urine when you cough or sneeze to having an urge to urinate that's so sudden and strong you don't get to a toilet in time. If urinary incontinence affects your daily activities, don't hesitate to see your doctor. For most people, simple lifestyle changes or medical treatment can ease discomfort or stop urinary incontinence
Waklert 150mg is known as the ultimate cognitive enhancer for amplifying productivity. With Waklert, unlock your entire mental capability and let magic begin. Full of benefits and laboriously crafted with precision, this invaluable supplement is what was missing in your life. Waklert 150mg is a commonly prescribed medicine for those persons who want to feel more alert and concentrated for long periods. Waklert, with its active ingredient Armodafinil, helps promote wakefulness. This medication does wonders by stimulating activity in the brain and keeping you vigilant and sharp throughout the day. You will experience a huge boost in productivity along with mental clarity once Waklert unleashes your brain's potential. It enhances the information retaining capability to the fullest within you, and you are able to absorb like a sponge so that you deliver the best output at any given task or project. Always be ahead, never miss deadlines, and put in the best possible levels of performance at work and studies. Not only will Waklert keep your cognitive faculties at their best, but the medicine also keeps you very positive, eliminating fatigue. Say goodbye to sluggishness and hello to a more energetic and rejuvenated self. Stay motivated for a longer time and create a sense of well-being, that too leading you to achieve your goals with unmatched determination. Be rest assured that Waklert is manufactured according to the highest standard in which safety and efficacy will be guaranteed.Buy Waklert 150mg online at our web store https://www.firstchoicemedss.c....om/waklert-150mg.htm