Top videos
Acanthamoeba keratitis is a rare disease in which amoebae invade the cornea of the eye. It may result in permanent visual impairment or blindness.
Back Massage
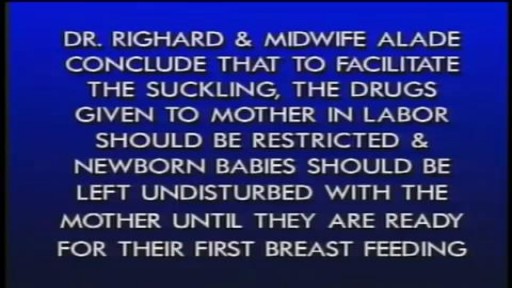
The importance of uninterrupted contact between mother and newborn SHOW MORE
Alone we can do so little; Together, we can do so much!
.
The team of RG Aesthetics brings to you the first-ever #gynecomastiacommunity in India! An Initiative for Patient Education and Interaction.
Dealing with Gynecomastia could be very challenging. People suffering from this issue are not able to enjoy many things that most of us take for granted like swimming, wearing tight-fitting T-Shirts, or being intimate with someone. These problems could lower their self-esteem.
The purpose of this community is to help provide people suffering from #gynecomastia an opportunity to talk out their worries and fear with surgeons and patients while educating and empowering them to make an informed decision.
Here’s why you must be a part of this community –
✓ Interact with Board Certified Surgeons and Patient community
✓ View Before-and-After patient results
✓ Connect with erstwhile patients who have now fully recovered
Fearing is not a solution. To defeat a problem, we must face it head-on!
Join our Gynecomastia Community Today!
Be a part of our Gynecomastia community.
✅ Get insights from our patient community
✅ Ask our board-certified plastic surgeons anything
✅ View the before-and-after patients' results
✅ Connect with other patients & ask them about their experience
✅ First of its a kind initiative in INDIA for patient education and interaction
Join our community: https://drrajatgupta.com/community/
Gynecomastia Helpline: +91 95689 99333
_______________________________________
About Dr. Rajat Gupta and RG Aesthetics
At RG Aesthetics, India’s best plastic surgeon, Dr. Rajat Gupta is at your service! With 10 years of experience, bord-certification, and international recognition, Dr. Gupta is the solution to all your contouring needs.
His expertise in liposuction techniques combined with the state-of-the-art technology available at RG Aesthetics ensures we continue providing the most reliable services with incredible, instantaneous results!
Our equipment allows for every kind of liposuction there is – especially the minimal invasive kinds. Dr Gupta reflects RG Aesthetics’ belief of the patient’s comfort always being paramount. Procedures at RG Aesthetics, under Dr Rajat Gupta, minimize trauma and speed up recovery time for the best results!
For more information please visit our website: https://drrajatgupta.com/
For more details,
contact us: 91-9251-711-711 or contact@drrajatgupta.com
Absence seizures involve brief, sudden lapses of consciousness. They're more common in children than adults. Someone having an absence seizure may look like he or she is staring into space for a few seconds. This type of seizure usually doesn't lead to physical injury. Absence seizures usually can be controlled with anti-seizure medications. Some children who have them also develop other seizures. Many children outgrow absence seizures in their teens.
A tummy tuck, also known as abdominoplasty, removes excess fat and skin and restores weakened muscles to create a smoother, firmer abdominal profile. But What is High Definition Abdominoplasty/Tummy Tuck? Watch Dr Rajat Gupta explaining about High Definition of Abdominoplasty/Tummy Tuck.
High Definition Abdominoplasty/Tummy Tuck is the latest advancement in tummy tuck surgeries. This not only entails tightening the skin but also enhances the shape and also gives a nice hourglass shape. The high-definition tummy tuck combines two advanced techniques related to the abdominal region — tummy tuck and high-definition liposuction (i.e. abdominal etching). The tummy tuck procedure aims to restore a flat and firm tummy by repairing muscle separation and removing sagging skin, whereas the abdominal etching technique aims to highlight the abdominal muscles with advanced liposuction techniques, producing the external appearance of toned abs.
Benefits of High-Definition Tummy Tuck:
-Provides a more sculpted physique than traditional tummy tucks
-Natural belly button design with more hidden incisions
-Low placement of tummy tuck, easily concealed with underwear
-Tightens your tummy skin
-Tightens stretched abdominal muscles
-Highlights your ab muscles
-Creates an hourglass shape with a narrower waist
_______________________________________
About Dr Rajat Gupta and RG Aesthetics
At RG Aesthetics, India’s best plastic surgeon, Dr Rajat Gupta is at your service! With 10 years of experience, brand-certification, and international recognition, Dr Gupta is the solution to all your contouring needs.
His expertise in liposuction techniques combined with the state-of-the-art technology available at RG Aesthetics ensures we continue providing the most reliable services with incredible, instantaneous results!
Our equipment allows for every kind of liposuction there is – especially the minimal invasive kinds. Dr Gupta reflects RG Aesthetics’ belief of the patient’s comfort always being paramount. Procedures at RG Aesthetics, under Dr Rajat Gupta, minimize trauma and speed up recovery time for the best results!
For more information please visit our website: https://www.drrajatgupta.com/
For more details,
contact us:+91-9251-711-711 or contact@drrajatgupta.com
#hdtummytuck #abdominoplasty #lipoabdominoplasty #plasticsurgeon #drrajatgupta
Waklert 150mg is known as the ultimate cognitive enhancer for amplifying productivity. With Waklert, unlock your entire mental capability and let magic begin. Full of benefits and laboriously crafted with precision, this invaluable supplement is what was missing in your life. Waklert 150mg is a commonly prescribed medicine for those persons who want to feel more alert and concentrated for long periods. Waklert, with its active ingredient Armodafinil, helps promote wakefulness. This medication does wonders by stimulating activity in the brain and keeping you vigilant and sharp throughout the day. You will experience a huge boost in productivity along with mental clarity once Waklert unleashes your brain's potential. It enhances the information retaining capability to the fullest within you, and you are able to absorb like a sponge so that you deliver the best output at any given task or project. Always be ahead, never miss deadlines, and put in the best possible levels of performance at work and studies. Not only will Waklert keep your cognitive faculties at their best, but the medicine also keeps you very positive, eliminating fatigue. Say goodbye to sluggishness and hello to a more energetic and rejuvenated self. Stay motivated for a longer time and create a sense of well-being, that too leading you to achieve your goals with unmatched determination. Be rest assured that Waklert is manufactured according to the highest standard in which safety and efficacy will be guaranteed.Buy Waklert 150mg online at our web store https://www.firstchoicemedss.c....om/waklert-150mg.htm
A needle is inserted into a joint for two main indications: aspiration of fluid (arthrocentesis) for diagnosis or for relief of pressure, or injection of medications. In practical terms, most injections into joints consist of a glucocorticoid, a local anesthetic, or a combination of the two. Occasionally saline is injected into the joint to diagnose a joint injury. This topic will review the basic technique of inserting a needle into a joint and the main indications for intraarticular steroid injections. The same techniques apply for injection of the less commonly used hyaluronate viscosupplementation agents into knees, hips, and perhaps shoulders.
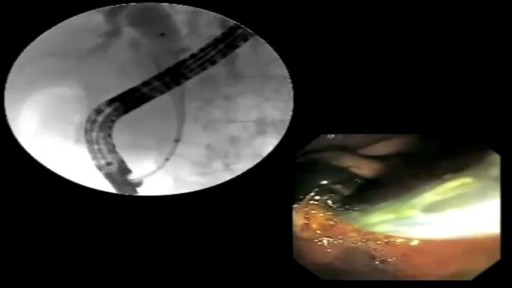
The placement of a percutaneous expandable biliary endoprosthesis was first reported in 1985 by Carrasco et al. in a canine model,[1] and the endoscopic placement of expandable metal stents to relieve biliary strictures in patients was first described in 1989.[2,3] Over the past two decades, the endoscopic approach to biliary endoprosthesis placement has largely supplanted the percutaneous approach. Self-expanding metal stents (SEMS) have traditionally been used for palliation of obstructive jaundice in patients with unresectable pancreaticobiliary tumors. However, SEMS are increasingly being used in patients with resectable cancers[4] and benign biliary strictures.[5] Uncovered SEMS (uSEMS) have been shown to have longer patency periods than plastic stents when used for malignant biliary obstruction and to be cost effective if the patient's life expectancy is greater than 4–6 months.[6–8] The common causes of malignant biliary obstruction are pancreatic cancer and cholangiocarcinoma.[9–11] Biliary drainage prior to surgical resection is controversial; several investigators have reported it to be beneficial owing to the improved tissue healing with reduced bilirubin levels,[12,13] but others have also reported its deleterious effects secondary to the additional intervention..
Erex 100mg is a very common product on sale in the market to cure Ed or impotency in men. sildenafil citrate (100 mg) serves as the prime active ingredient which is employed in the formulation of the medicine. Ed is a condition where a man is unable to reach firm erection sufficient for the intercourse which is a very big issue so erex 100mg can raise the blood towards the genital organ of male and helps them to get firm erection sufficient for the intercourse.You must avoid fatty meal prior to the intake of this medicine.You can buy Erex 100mg tablets online in Australia. This is not an everyday usage medicine which you can use.Anyways, you can take this thirty minutes or one hour before intercourse so that it has to show its effective performance.With the flow of time it will try to improve your performance and will give you more satisfaction.Keep it out of your children and pets(if any) reach. Keep it in a dry and cool place away from the moisture.Buy Erex 100mg online at our web store https://www.firstchoicemedss.com/erex-100mg.html
Sildigra Black Force is a potent medicine that works efficiently to enhance improvement in erectile dysfunction. It comes with an active substance of Sildenafil 200mg.
Buy Now : https://www.rsmenterprises.in/....product/viewdetail/s
#rsmenterprises #health #healthcare #sildigrablackforce #sildenafil200mg #edmedicine #genericviagra200mg #maleedmedicine
In caring for patients who are critically ill, access to the central venous circulation is important. Central venous access allows the placement of various types of intravenous (IV) lines to facilitate the infusion of fluids, blood products, and drugs and to obtain blood for laboratory analysis. It is also an essential procedure in patients in whom placement of a line in a peripheral vein is impossible. A central line may be the only means of venous access in such cases.
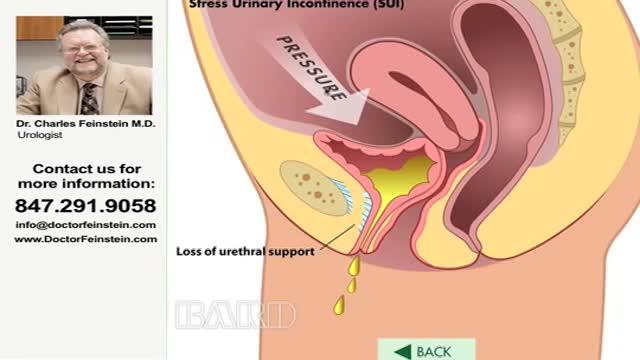
Urinary incontinence — the loss of bladder control — is a common and often embarrassing problem. The severity ranges from occasionally leaking urine when you cough or sneeze to having an urge to urinate that's so sudden and strong you don't get to a toilet in time. If urinary incontinence affects your daily activities, don't hesitate to see your doctor. For most people, simple lifestyle changes or medical treatment can ease discomfort or stop urinary incontinence
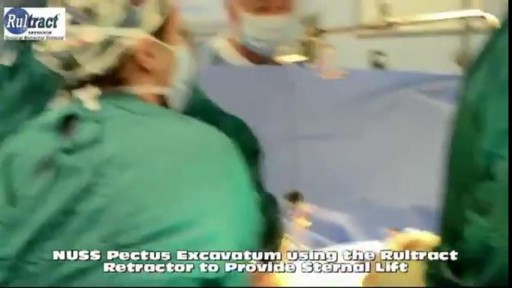
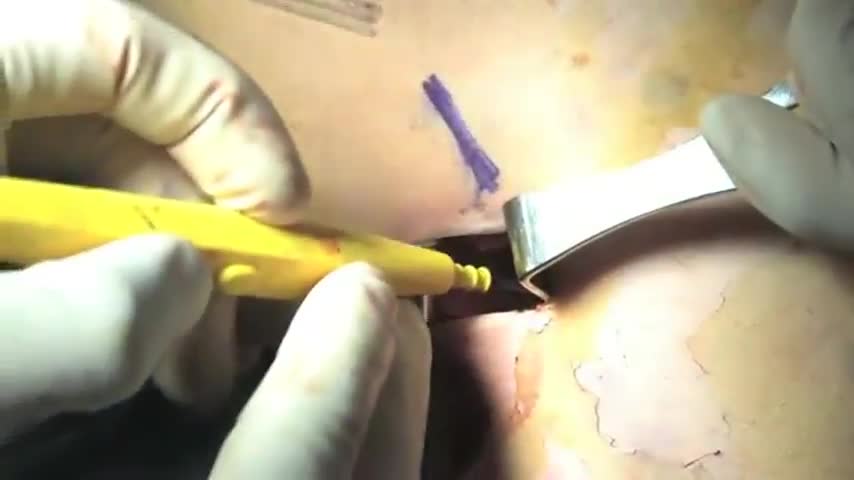
Pectus excavatum repair is surgery to correct pectus excavatum. This is a congenital (present at birth) deformity of the front of the chest wall that causes a sunken breastbone (sternum) and ribs. Pectus excavatum is also called funnel or sunken chest. It may worsen during the teen years.
Tadalafil Super Active Tablets are used to treat the physical problems of erectile dysfunction in men. These oral drugs are effectively used in the treatment for ED disorders in men assuring erection for longer duration of time.
Buy Now : https://www.rsmenterprises.in/....product/viewdetail/t
#rsmenterprises #health #healthcare #tadagrasuperactive #tadalafil20mg #genericcialis #malecialis
Without a doubt, Caverta 100mg is the best solution to lead a good and healthy personal life. An extraordinary medication, Caverta 100mg is designed to overcome all issues of ED in you and help regain your sensual power and general quality of life. You can buy Caverta 100mg tablets online in Australia.This powerful formulation Caverta 100mg and its proven track record have made it an ideal companion for men seeking a reliable and efficient drug. The active elements of Sildenafil citrate present in this effective medicine relax the muscles and increase blood flow in the penile area to ensure that a firm and long-lasting erection is achieved. Every pill is well produced with utmost diligence in order to ensure proper dosage and quick response. Caverta 100mg has empowered you to enjoy spontaneous, fulfilling lovemaking whenever the urge strikes, thus leaving anxieties and frustration of ED in the dust. A phenomenal reliability and safety record are what make Caverta 100mg really stand out from the rest of drugs. Now, you can comfortably explore sensual needs without the fear of performance failures with Caverta 100mg. Take this golden opportunity to have intimate times with your partner at your discretion. Caverta 100mg enables you to again feel the thrill of spontaneous lovemaking and take your love and emotional connections to a higher level.Buy Caverta 100mg online at our web store https://www.firstchoicemedss.c....om/caverta-100mg.htm
Diabetes, often referred to by doctors as diabetes mellitus, describes a group of metabolic diseases in which the person has high blood glucose (blood sugar), either because insulin production is inadequate, or because the body's cells do not respond properly to insulin, or both. Patients with high blood sugar will typically experience polyuria (frequent urination), they will become increasingly thirsty (polydipsia) and hungry (polyphagia).
After pregnancy, there are a lot of women who need Tummy Tuck Surgery or Abdominoplasty. Likewise, there are also many men who need this surgery who have lost weight and have saggy skin. These men and women may be very apprehensive about the recovery after the surgery. In this video, Dr. Rajat Gupta (Cosmetic plastic surgeon) will guide us about this topic.
Abdominoplasty or Tummy Tuck Surgery Time -
The most important concern of the people who are considering this surgery is about recovery. Tummy Tuck Surgery or Abdominoplasty needs 2-3 hours for the surgery depending upon the extent of your fat. It is preferred usually to do a 360 liposuction.
Abdominoplasty or Tummy Tuck Surgery Recovery Time -
After the surgery, the patient stays 1 night or sometimes 2 nights in the hospital, but they start walking the same way. For the first 10-12 days walk with a slight bend so that your scar near to your bikini doesn't stretch. From the very next day, you can do your basic things at home like walking around, having food on your own, etc.
First 3-4 days there is a little pain and tightness in the patient. After 3-4 days, they start recovering well and the discomfort is much lesser. Every individual recovers differently as their pain threshold is different. Everyone has a different strength.
You can resume your job in 7-10 days. However, if your job has more physical work then they can resume in 15 days. You can resume your cardio exercises like running, jogging after 3-4 weeks. This is the basic timeline for recovery.
Antibiotics are given for the first 7 days. The dressing is removed after 3 days. After 7 days you are allowed to apply scar creams so that the scar becomes light enough.
To know more watch the full video.
If you have any regarding this topic you can ask us in the comment section.
_______________________________________
About Dr. Rajat Gupta and RG Aesthetics
At RG Aesthetics, India’s best plastic surgeon, Dr. Rajat Gupta is at your service! With 10 years of experience, brand certification, and international recognition, Dr. Gupta is the solution to all your contouring needs.
His expertise in liposuction techniques combined with the state-of-the-art technology available at RG Aesthetics ensures we continue providing the most reliable services with incredible, instantaneous results!
Our equipment allows for every kind of liposuction there is – especially the minimal invasive kinds. Dr Gupta reflects RG Aesthetics’ belief of the patient’s comfort always being paramount. Procedures at RG Aesthetics, under Dr Rajat Gupta, minimize trauma and speed up recovery time for the best results!
For more information please visit our website: https://drrajatgupta.com/
For more details,
contact us: 91-9251-711-711 or contact@drrajatgupta.com
#tummytuck #drrajatgupta #rgaesthetics
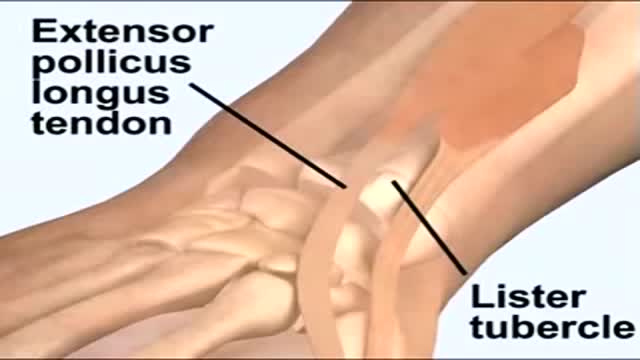
Biceps tenodesis is a common procedure performed for tendinopathy of the long head of the biceps brachii (LHB). Indications include partial-thickness LHB tear, tendon subluxation with or without subscapularis tear, and failed conservative management of bicipital tenosynovitis. Biceps tenodesis may also be performed for superior labrum anterior to posterior tears.
How Does a Bone Heal? All broken bones go through the same healing process. This is true whether a bone has been cut as part of a surgical procedure or fractured through an injury. The bone healing process has three overlapping stages: inflammation, bone production and bone remodeling. Inflammation starts immediately after the bone is fractured and lasts for several days. When the bone is fractured, there is bleeding into the area, leading to inflammation and clotting of blood at the fracture site. This provides the initial structural stability and framework for producing new bone. Diagram of inflammation in a fractured bone Bone production begins when the clotted blood formed by inflammation is replaced with fibrous tissue and cartilage (known as soft callus). As healing progresses, the soft callus is replaced with hard bone (known as hard callus), which is visible on x-rays several weeks after the fracture. Bone remodeling, the final phase of bone healing, goes on for several months. In remodeling, bone continues to form and becomes compact, returning to its original shape. In addition, blood circulation in the area improves. Once adequate bone healing has occurred, weightbearing (such as standing or walking) encourages bone remodeling.