Top Videos

Neonatal resuscitation skills are essential for all health care providers who are involved in the delivery of newborns. The transition from fetus to newborn requires intervention by a skilled individual or team in approximately 10% of all deliveries. This figure is concerning because 81% of all babies in the United States are born in nonteaching, nonaffiliated level I or II hospitals. In such hospitals, the volume of delivery service may not be perceived as sufficient economic justification for the continuous in-hospital presence of personnel with high-risk delivery room experience, as recommended by the American Academy of Pediatrics (AAP) and the American College of Obstetricians and Gynecologists (ACOG). [1] Perinatal asphyxia and extreme prematurity are the 2 complications of pregnancy that most frequently necessitate complex resuscitation by skilled personnel. However, only 60% of asphyxiated newborns can be predicted ante partum. The remaining newborns are not identified until the time of birth. Additionally, approximately 80% of low-birth-weight infants require resuscitation and stabilization at delivery. Nearly one half of newborn deaths (many of which involve extremely premature infants) occur during the first 24 hours after birth. Many of these early deaths also have a component of asphyxia or respiratory depression as an etiology. For the surviving infants, effective management of asphyxia in the first few minutes of life may influence long-term outcome. Even though prenatal care can identify many potential fetal difficulties ante partum, allowing maternal transfer to the referral center for care, many women who experience preterm labor are not identified prospectively and therefore are not appropriately transferred to a tertiary perinatal center. Consequently, many deliveries of extremely premature infants occur in smaller hospitals. For this reason, all personnel involved in delivery room care of the newborn should be trained adequately in all aspects of neonatal resuscitation. Additionally, equipment that is appropriately sized to resuscitate infants of all gestational ages should be available in all delivering institutions, even if the institution does not care for preterm or intensive care infants. Along with the necessary skills, the practitioner should approach any resuscitation with a good comprehension of transitional physiology and adaptation, as well as an understanding of the infant's response to resuscitation. Resuscitation involves much more than possessing an ordered list of technical skills and having a resuscitation team; it requires excellent assessment skills and a grounded understanding of physiology.
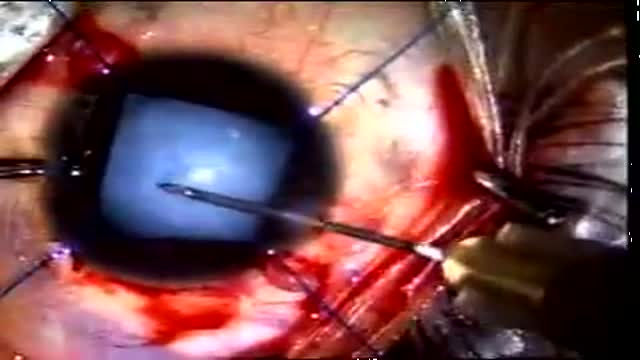
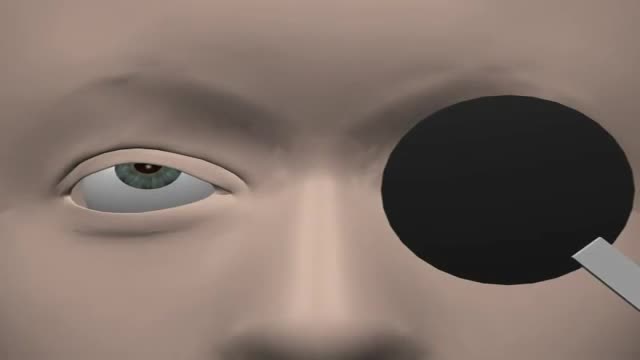
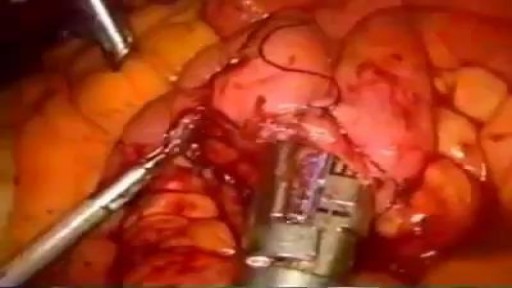
This video shows management of rupture of the posterior capsule post blunt trauma in a child aged 8. Pre-operative suspicion of PCR was strong because of a flat anterior. So we were careful in our approach from the very beginning. CCC was performed and then dry aspiration of lens matter initiated. Sice vitreous showed, so anterior vitrectomy was done along with systematic removal of the lens matter. An acrysof multi-component lens was implanted into the sulcus and optic captured into the CCC.Outcome was very good.

Ganglion cysts are the most common mass or lump in the hand. They are not cancerous and, in most cases, are harmless. They occur in various locations, but most frequently develop on the back of the wrist. These fluid-filled cysts can quickly appear, disappear, and change size.

Skin grafting is a type of medical grafting involving the transplantation of skin. The transplanted tissue is called a skin graft. Skin grafting is often used to treat: Extensive wounding or trauma Burns Areas of extensive skin loss due to infection such as necrotizing fasciitis or purpura fulminans Specific surgeries that may require skin grafts for healing to occur – most commonly removal of skin cancers. Skin grafts are often employed after serious injuries when some of the body’s skin is damaged. Surgical removal (excision or debridement) of the damaged skin is followed by skin grafting. The grafting serves two purposes: it can reduce the course of treatment needed (and time in the hospital), and it can improve the function and appearance of the area of the body which receives the skin graft. There are two types of skin grafts, the more common type is where a thin layer is removed from a healthy part of the body (the donor section), like peeling a potato, or a full thickness skin graft, which involves pitching and cutting skin away from the donor section. A full thickness skin graft is more risky, in terms of the body accepting the skin, yet it leaves only a scar line on the donor section, similar to a Cesarean section scar. For full thickness skin grafts, the donor section will often heal much more quickly than the injury and is less painful than a partial thickness skin graft.