סרטונים מובילים

The peroneal artery is closely positioned to the fibula. The artery arises from the tibioperoneal trunk, distal to the takeoff of the anterior tibial artery (seen in the illustration below perforating the interosseous membrane). The peroneal artery sends perforators laterally to the skin of the lower leg, sometimes in a septocutaneous fashion via the lateral intermuscular septum, but often with muscular perforators. The length of the pedicle is usually short, but can be increased substantially by dissecting the peroneal artery and its venae from the fibula and using the distal bone for reconstruction.

We will show how to know if you have a sports hernia. These are a few tests you can do on your own. Lower abdominal pain and tightness that increases with twisting and kicking. Stretching and exercises tend to make the discomfort increase.
Want more info? We have a free webinar that covers hip, groin, adductor, lower abdominal strains and sports hernia diagnosis in detail. Use this link to get access. https://bit.ly/37thtNF
#sportshernia #hernia #hippain
To work with us, contact us using this link https://bit.ly/3zCBnzZ or call us 714-502-4243. We have online programs, virtual and in-person options.
Costa Mesa, CA www.p2sportscare.com
Option 1: Groin On-Demand Webinar https://bit.ly/37thtNF
Option 2: Video Guide https://bit.ly/33aLIqC
Option 3 (the best): Work With Us https://www.p2sportscare.com/
Sports Hernia Diagnosis
What Is A Sports Hernia?
A sports hernia is tearing of the transversalis fascia of the lower abdominal or groin region. A common misconception is that a sports hernia is the same as a traditional hernia. The mechanism of injury is rapid twisting and change of direction within sports, such as football, basketball, soccer and hockey.
The term “sports hernia” is becoming mainstream with more professional athletes being diagnosed. The following are just to name a few:
Torii Hunter
Tom Brady
Ryan Getzlaf
Julio Jones
Jeremy Shockey
If you follow any of these professional athletes, they all seem to have the same thing in common: Lingering groin pain. If you play fantasy sports, this is a major headache since it seems so minor, but it can land a player on Injury Reserve on a moments notice. In real life, it is a very frustrating condition to say the least. It is hard to pin point, goes away with rest and comes back after activity, but is hardly painful enough to make you want to stop. It lingers and is always on your mind. And if you’re looking for my step-by-step sports hernia rehab video course here it is.
One the best definitions of Sport hernias is the following by Harmon:
The phenomena of chronic activity–related groin pain that it is unresponsive to conservative therapy and significantly improves with surgical repair.”
This is truly how sports hernias behave in a clinical setting. It is not uncommon for a sports hernia to be unrecognized for months and even years. Unlike your typical sports injury, most sports medicine offices have only seen a handful of cases. It’s just not on most doctors’ radar. The purpose of this article is not only to bring awareness about sports hernias, but also to educate.
Will you find quick fixes in this article for sports hernia rehab?
Nope. There is no quick fix for this condition, and if someone is trying to sell you one, they are blowing smoke up your you-know-what.
Is there a way to decrease the pain related to sports hernias?
Yes. Proper rehab and avoidance of activity for a certain period of time will assist greatly, but this will not always stop it from coming back. Pain is the first thing to go and last thing to come. Do not be fooled when you become pain-free by resting it. Pain is only one measure of improvement in your rehab. Strength, change of direction, balance and power (just to name a few) are important, since you obviously desire to play your sport again. If you wanted to be a couch potato, you would be feeling better in no time. Watching Sports Center doesn’t require any movement.
Why is this article so long?
There is a lot of information on sports hernias available to you on the web. However, much of the information is spread out all over the internet and hard for athletes to digest due to complicated terminology. This article lays out the foundational terminology you will need to understand what options you have with your injury. We will go over anatomy, biomechanics, rehab, surgery, and even the fun facts. The information I am using is from the last ten years of medical research, up until 2016. We will be making updates overtime when something new is found as well. So link to this page and share with friends. This is the best source for information on sports hernias you will find.
Common Names (or Aliases?) for Sports Hernias
Sportsman’s Hernia
Athletic Pubalgia
Gilmore’s Groin
How Do You Know If You Have A Sports Hernia?
Typical athlete characteristics:
Male, age mid-20s
Common sports: soccer, hockey, tennis, football, field hockey
Motions involved: cutting, pivoting, kicking and sharp turns
Gradual onset
How A Sports Hernia Develops
Chronic groin pain typically happens over time, which is why with sports hernias, we do not hear many stories of feeling a “pop” or a specific moment of injury. It is the result of “overuse” mechanics stemming from a combination of inadequate strength and endurance, lack of dynamic control, movement pattern abnormalities, and discoordination of motion in the groin area.

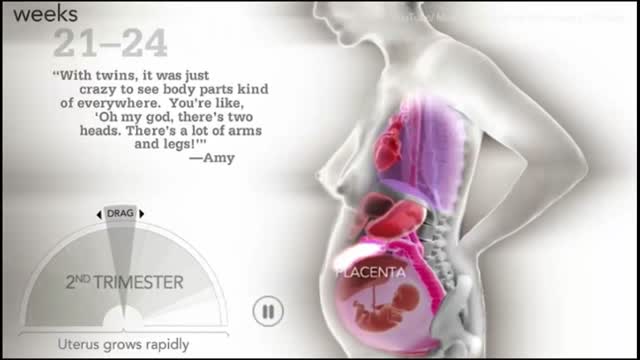
Your baby is still tiny, but already your body is changing. Your breasts start to swell and may feel tender. Tiredness, nausea, and a frequent need to pee are common pregnancy symptoms. In your second trimester, your growing uterus gradually rises up out of your pelvis.
People with serious comprehension difficulties have what is called Wernicke’s aphasia and: Often say many words that don’t make sense. May fail to realize they are saying the wrong words; for instance, they might call a fork a “gleeble.” May string together a series of meaningless words that sound like a sentence but don’t make sense. Have challenges because our dictionary of words is shelved in a similar region of the left hemisphere, near the area used for understanding words.
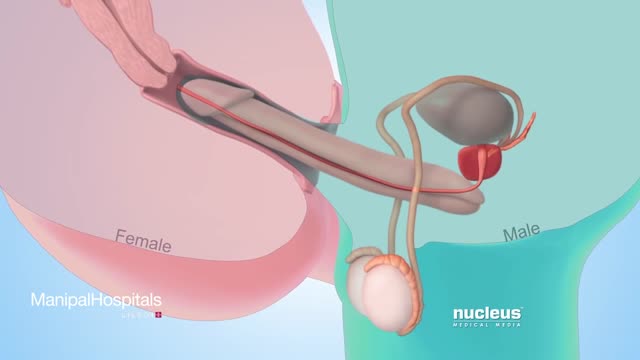
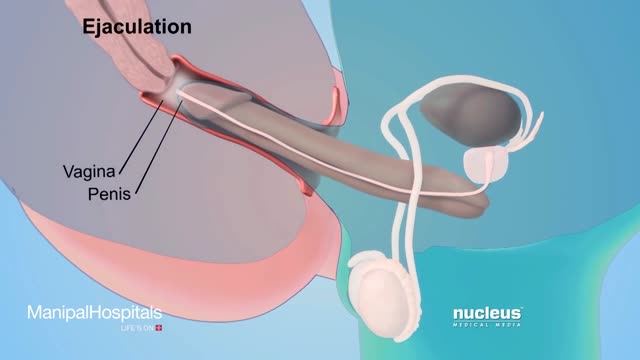
Testicular sperm aspiration (TESA) is a procedure performed for men who are having sperm retrieved for in vitro fertilization/intracytoplasmic sperm injection (IVF/ICSI). It is done with local anesthesia in the operating room or office and is coordinated with their female partner's egg retrieval.

Classical PKU is an autosomal recessive disorder, caused by mutations in both alleles of the gene for phenylalanine hydroxylase (PAH), found on chromosome 12. In the body, phenylalanine hydroxylase converts the amino acid phenylalanine to tyrosine, another amino acid.