Najbolji videi

MUSC Children’s Health offers South Carolina’s only Level 1 Children’s Surgery Center, representing excellence in inpatient surgery at MUSC Shawn Jenkins Children’s Hospital, as well as outpatient surgery at R. Keith Summey Medical Pavilion. These two state-of-the-art facilities are equipped with a team of pediatric board-certified providers utilizing pediatric-specific devices and the most technologically advanced tools.
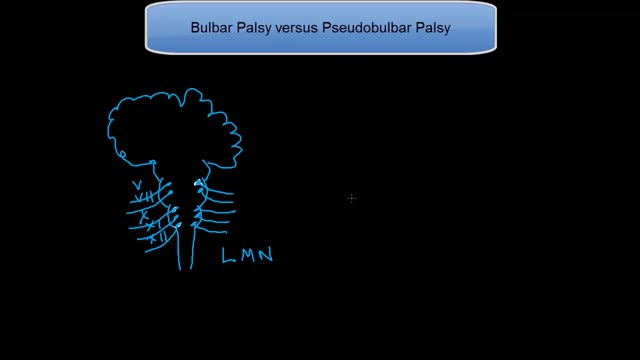
People with serious comprehension difficulties have what is called Wernicke’s aphasia and: Often say many words that don’t make sense. May fail to realize they are saying the wrong words; for instance, they might call a fork a “gleeble.” May string together a series of meaningless words that sound like a sentence but don’t make sense. Have challenges because our dictionary of words is shelved in a similar region of the left hemisphere, near the area used for understanding words.

http://control-blood-sugar.good-info.co Low Blood Sugar, Signs Of Low Blood Sugar, Low Iron In Blood, Normal Glucose Levels In Blood Are You Suffering From High Or Uncontrollable Blood Sugar? Because This May Be The Solution. If you’re one of the 387 million people in the world trying to win the battle against uncontrollable blood sugar or even diabetes. Then you’re in the right place, as believe it or not, these conditions can be completely reversed from the comfort of your own home in just 3 short weeks. Are you. Tired of poking your skin with expensive needles everyday? Tired of dealing with the constant lethargy and lack of energy that’s associated with your uncontrollable blood sugar? Tired of living your life with stubborn body fat on your waist, legs,and thighs? Tired of being embarrassed to go to the beach or even taking your shirt off in front of your kids? Tired of waking up with a headache in a soaked bed from sweating so much at night? If you are sick and tired of these all of these conditions and more, then I am happy to tell you that all these conditions of your uncontrollable blood sugar can be completely thrown away for good! click here. http://control-blood-sugar.good-info.co

Hysteroscopy is a procedure that allows your doctor to look inside your uterus in order to diagnose and treat causes of abnormal bleeding. Hysteroscopy is done using a hysteroscope, a thin, lighted tube that is inserted into the vagina to examine the cervix and inside of the uterus.
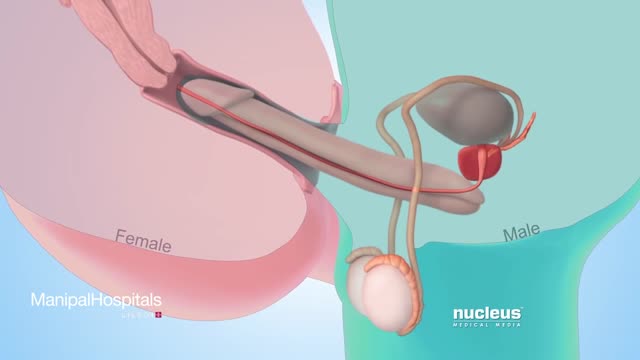
Testicular sperm aspiration (TESA) is a procedure performed for men who are having sperm retrieved for in vitro fertilization/intracytoplasmic sperm injection (IVF/ICSI). It is done with local anesthesia in the operating room or office and is coordinated with their female partner's egg retrieval.
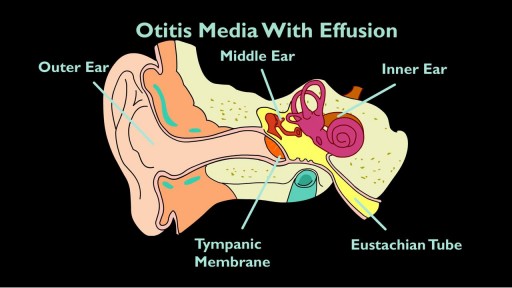
The eustachian tube drains fluid from your ears to the back of your throat. If it clogs, otitis media with effusion (OME) can occur. If you have OME, the middle part of your ear fills with fluid, which can increase the risk of ear infection. OME is very common. According to the Agency of Healthcare Research and Quality, about 90 percent of children will have OME at least once by the age of 10.

Classical PKU is an autosomal recessive disorder, caused by mutations in both alleles of the gene for phenylalanine hydroxylase (PAH), found on chromosome 12. In the body, phenylalanine hydroxylase converts the amino acid phenylalanine to tyrosine, another amino acid.