ویدیوهای برتر

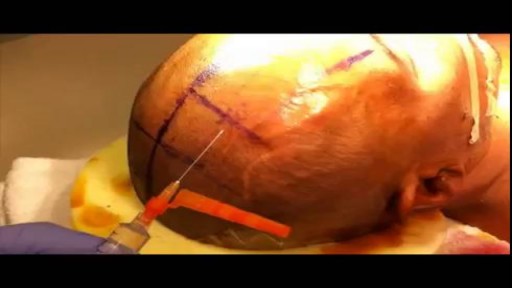
This video shows Prof Dan Reinstein, MD MA(Cantab) FRCSC DABO FRCOphth FEBO performing a ReLEx SMILE keyhole LASIK procedure using the latest surgical instrument that he helped to develop (Malosa MMSU1297 - Reinstein Lenticule Separator: http://www.malosa.com/en/reinstein-le...). This instrument enables the procedure to be performed with one instrument, through one 2mm incision, using only one sweep per plane, and taking about 30 seconds to separate and withdraw the lenticule, improving day 1 uncorrected vision over other lenticule extraction techniques that require more corneal manipulation.
Water is an essential nutrient for the body, as the body loses water through perspiration, breathing, bowel movements, and in urine. Water must be consumed regularly to maintain a sufficient level. Water has many vital functions in the body, including… Serving as a lubricant. Water is a main component of saliva, which helps moisten food making it easier to swallow. Water also helps lubricate joints, reducing friction and inflammation. Water is important in body temperature regulation. When body heat rises, such as during strenuous activities, the body starts to sweat to cool itself. And sweat is made up almost entirely of water.
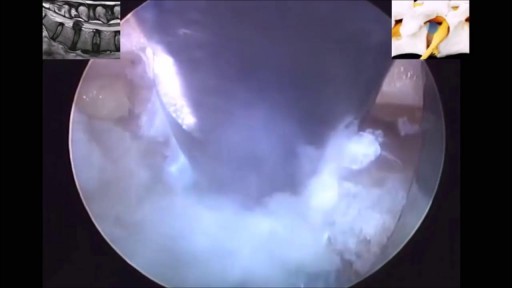
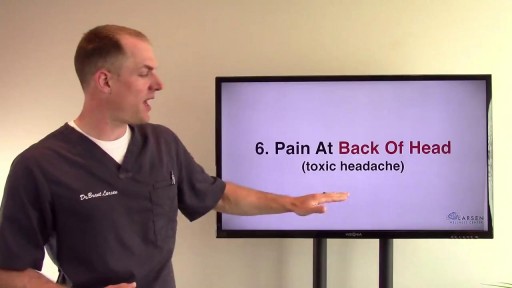
If you have been diagnosed with a bulging disc, you are not alone. Bulging discs, also known as a disc protrusion, are a very common occurrence. They usually remain asymptomatic; however, they can cause discomfort and disability in various parts of the body if the disc compresses an adjacent nerve root or the spinal cord. As we age, the outer fibrous portion of our discs can weaken. Pressure from the central core of the disc can then stretch to the outer rim, causing the disc to bulge. If left untreated, the disc can continue to bulge until it tears, which is classified as a herniated disc.
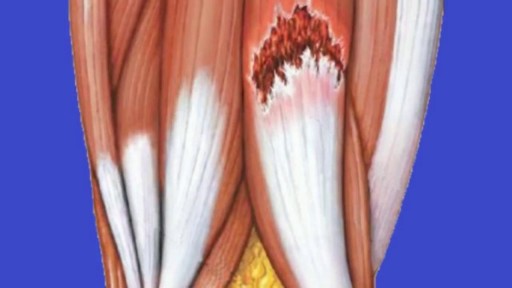
Pain in the upper thigh can be difficult to diagnose because this area of the body contains many muscles, tendons, and ligaments. This kind of pain may often be due to minor muscle injuries that are treatable at home. When the pain is intense or does not go away, however, it may signal a more serious problem. In this video, we examine some common causes of pain in the upper thigh, along with any symptoms that may occur alongside. We also take a look at the treatment options and how to prevent this type of pain.
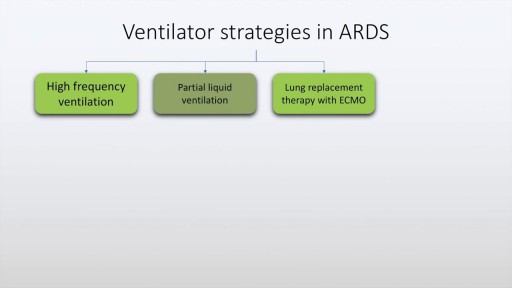
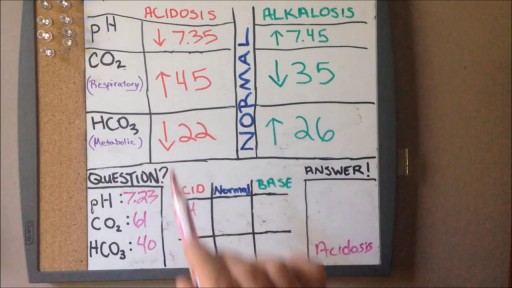
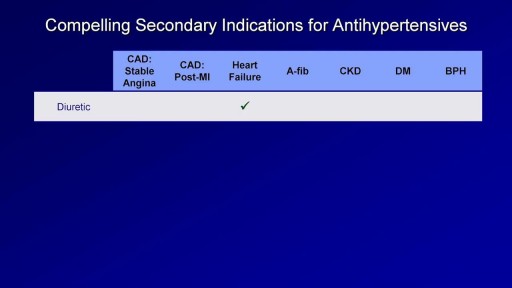
Acute respiratory distress syndrome is characterised by rapid onset dyspnea, bilateral infiltrates on chest x-ray and respiratory failure. This may be due to conditions which directly affect the lung such as pneumonia, aspiration and near drowning. It may also be due to indirect lung injury, as in conditions like sepsis, pancreatitis, trauma and poisoning. The diagnostic criteria of ARDS, often described as the Berlin criteria is discussed in this presentation along with various management aspects of ARDS including ventilation strategies and use of antibiotics and diuretics. Finally prognostic features and alternative strategies are also discussed.
A detailed description of Adrenal insufficiency (Addison's disease) including basic physiology of the HPA axis, causes of primary and secondary insufficiency, clinical features of acute and chronic adrenal insufficiency. Lab testing for Addison's disease is also dealt with in detail. The management, both short term and long term are discussed in detail.

Every day, specialists deliver high-quality care in 68 disciplines in health centres across Canada. Yet many Canadians know very little about what many specialists actually do, and the important role these disciplines play in Canada’s health care system.

Tinnitus (TIN-ih-tus) is the perception of noise or ringing in the ears. A common problem, tinnitus affects about 1 in 5 people. Tinnitus isn't a condition itself — it's a symptom of an underlying condition, such as age-related hearing loss, ear injury or a circulatory system disorder

Acne can form several types of skin blemish, each with a distinct appearance and symptoms. Most minor acne blemishes respond to at-home care and over-the-counter medications. However, people with severe or long-term acne should speak with a doctor or dermatologist. Acne affects around 80 percent of adolescents and young adults. About 40–50 million Americans have acne at any given time. The following are common types of blemish associated with acne: whiteheads blackheads pustules, which are commonly called pimples papules cysts nodules Each type of acne lesion requires a different treatment. Receiving prompt, correct treatment can reduce the risk of long-term skin complications, such as dark spots and scarring. Acne blemishes fall into two categories, depending on whether or not they cause inflammation of the surrounding skin. Whiteheads Whiteheads Blackheads blackheads are pockets of oxidized melanin on the surface of the skin Papules Papules Pustules (pimples) Pustules (pimples) Nodules Nodules Cysts pus in a cyst 1of6 Noninflammatory acne types Whiteheads and blackheads are types of noninflammatory acne lesion. They are the least severe forms of acne. Noninflammatory blemishes usually do not cause swelling and are not very painful. Whiteheads The medical term for whiteheads is closed comedones. These are small, whitish or flesh-colored spots or bumps. They usually have a white, circular center surrounded by a red halo. A hair will sometimes emerge from the center of a whitehead, or it may appear to be trapped within the blemish. The skin around a whitehead may appear to be tight or wrinkled, especially when the whitehead is large or especially raised. ADVERTISEMENT Approved NSCLC Treatment - HCP Info & Resources Request A Rep & Discover A Therapy For Stage III NSCLC. www.stage-iii-nsclc-therapy.com Whiteheads typically do not cause scarring. Blackheads Blackheads are also called open comedones. They are small, black or dark-colored spots that may appear as slightly raised bumps. The skin around a blackhead usually appears normal, while the center of the blackhead is darker than the surrounding area. The coloration is not a result of trapped dirt. Blackheads are simply whiteheads that have opened and widened. When the contents of a whitehead are exposed to air, they darken. Treatment options Many over-the-counter rinses, moisturizers, gels, toners, and creams can treat noninflammatory acne blemishes. They often contain a mix of active ingredients. The following ingredients in over-the-counter treatments can help to break down whiteheads and blackheads: benzoyl peroxide salicylic acid sulfur resorcinol Also, several home remedies and lifestyle changes can help to reduce most minor-to-mild forms of noninflammatory acne. It may help to try: washing the face with lukewarm water and soap twice daily washing the whole body every 2 days reducing stress eating a healthful, balanced diet staying hydrated avoiding over-washing or irritating the skin limiting exposure to the sun always wearing sunscreen when outdoors People should never pop acne blemishes. Doing so can lead to complications, such as: nodules cysts scarring dark spots pitting Inflammatory acne types Inflammatory acne blemishes include: papules pustules nodules cysts Inflammatory acne is more severe than noninflammatory acne, and this type is more likely to cause complications, such as scarring or pitting. Blemishes or lesions that are inflamed, or red, swollen, and warm to the touch can result from inflammatory acne. Minor-to-mild forms Papules Papules are bumps under the skin's surface. They are solid, tender, pink, and raised, and the skin around a papule is usually slightly swollen and red. Unlike whiteheads, papules have no visible center. Unlike blackheads, the pores of a papule do not appear to be widened. Papules develop when whiteheads or blackheads cause so much irritation that they damage some of the surrounding skin. The damage leads to inflammation. Pustules (pimples) Pustules are larger, tender bumps with a defined circular center. The center is filled with whitish or yellowish pus, and the bump has a pink or red base. Immune cells and bacterial cells collect to form this pus. Pustules typically look like much larger and more inflamed whiteheads. Treatment options Several home remedies and over-the-counter medications can treat minor-to-mild papules and pustules. The following tips can help: washing the affected area with cool water and soap using clean hands or a clean, gentle facecloth twice a day applying a warm compress or cloth to the affected area for 10–15 minutes to encourage trapped debris to rise to the surface using products with benzoyl peroxide to combat bacteria using products with salicylic acid to remove dead skin cells and other debris How do you prevent pimples? How do you prevent pimples? How can you prevent pimples from forming? Learn 15 methods of prevention here, including home remedies, lifestyle changes, and diet tips. READ NOW Moderate-to-severe forms Nodules Nodules are hard, painful, inflamed lumps located deep within the skin. They look like larger, deeper papules and have no visible center or head. This type of acne lesion develops when clogged pores damage tissues and cells deep beneath the skin's surface. Nodules are a severe form of acne blemish, and they can cause skin complications such as dark spots or scarring. Cysts Cysts are very large, soft, painful, red or white lumps situated deep in the skin. They are filled with pus. Cysts form deeper within the skin than nodules, and they are the most severe type of acne blemish. Cysts can also cause skin complications, such as scarring. Treatment options People cannot treat moderate-to-severe inflammatory blemishes at home. These lesions require care from a doctor or dermatologist. The doctor can use many products and procedures to treat nodules and cysts. These include: antibiotics, such as tetracycline, doxycycline, and amoxicillin topical corticosteroids oral contraceptives for hormonal-related acne systematic retinoids, such as isotretinoin steroid injections chemical peels photodynamic therapy to combat bacteria drainage and extraction to remove large cysts What causes acne? young woman with forehead acne When a pore becomes clogged, acne can develop. Normally, dead cells collect in the skin's pores, then slowly rise to the surface of the openings and eventually fall away from the skin. A natural body oil called sebum helps to prevent skin cells from drying out. The glands that produce this oil are attached to the pores. When excess sebum builds up, it can cause dead cells to stick together, forming a mixture that becomes trapped in the pores. Acne occurs when a pore becomes clogged with dead skin cells, natural body oils, and a type of bacteria. These bacteria live on the skin and are called Propionibacterium acnes. If they enter and infect clogged pores, this causes acne blemishes to form. When to see a doctor In cases of minor-to-moderate acne, a person will generally have to use home and over-the-counter remedies consistently for 4–8 weeks before they see results. More severe inflammatory types of acne tend to take much longer to clear up. Speak to a doctor or dermatologist if whiteheads, blackheads, papules, or pustules: are severe do not respond to over-the-counter medications are very painful are very large bleed a lot release a lot of pus cover a significant portion of the face or body cause emotional distress develop very close to sensitive areas, such as the eyes or lips Most active ingredients in over-the-counter products are available in prescription-strength treatments. Dermatologists can also remove lesions that are very large or persistent. They can also remove those that do not respond to other forms of treatment. Always see a doctor or dermatologist about nodules and cysts, because these require medical care. Untreated nodules and cysts and those that have been picked or popped can cause scarring.