Top videos

New research from Mount Sinai Health System says these surgeries have limited effectiveness and can be economically unjustifiable when they're done on patients with less severe symptoms.
» Subscribe to NBC News: http://nbcnews.to/SubscribeToNBC
» Watch more NBC video: http://bit.ly/MoreNBCNews
NBC News is a leading source of global news and information. Here you will find clips from NBC Nightly News, Meet The Press, and original digital videos. Subscribe to our channel for news stories, technology, politics, health, entertainment, science, business, and exclusive NBC investigations.
Connect with NBC News Online!
Visit NBCNews.Com: http://nbcnews.to/ReadNBC
Find NBC News on Facebook: http://nbcnews.to/LikeNBC
Follow NBC News on Twitter: http://nbcnews.to/FollowNBC
Follow NBC News on Google+: http://nbcnews.to/PlusNBC
Follow NBC News on Instagram: http://nbcnews.to/InstaNBC
Follow NBC News on Pinterest: http://nbcnews.to/PinNBC
New Study Questions Effectiveness Of Knee Replacement Surgery | NBC Nightly News
An estimated 900,000 knee replacements are performed in the U.S. every year, but experts say about 15% of patients aren’t totally pleased with the outcome. An advancement in technology is focused on improving those outcomes.

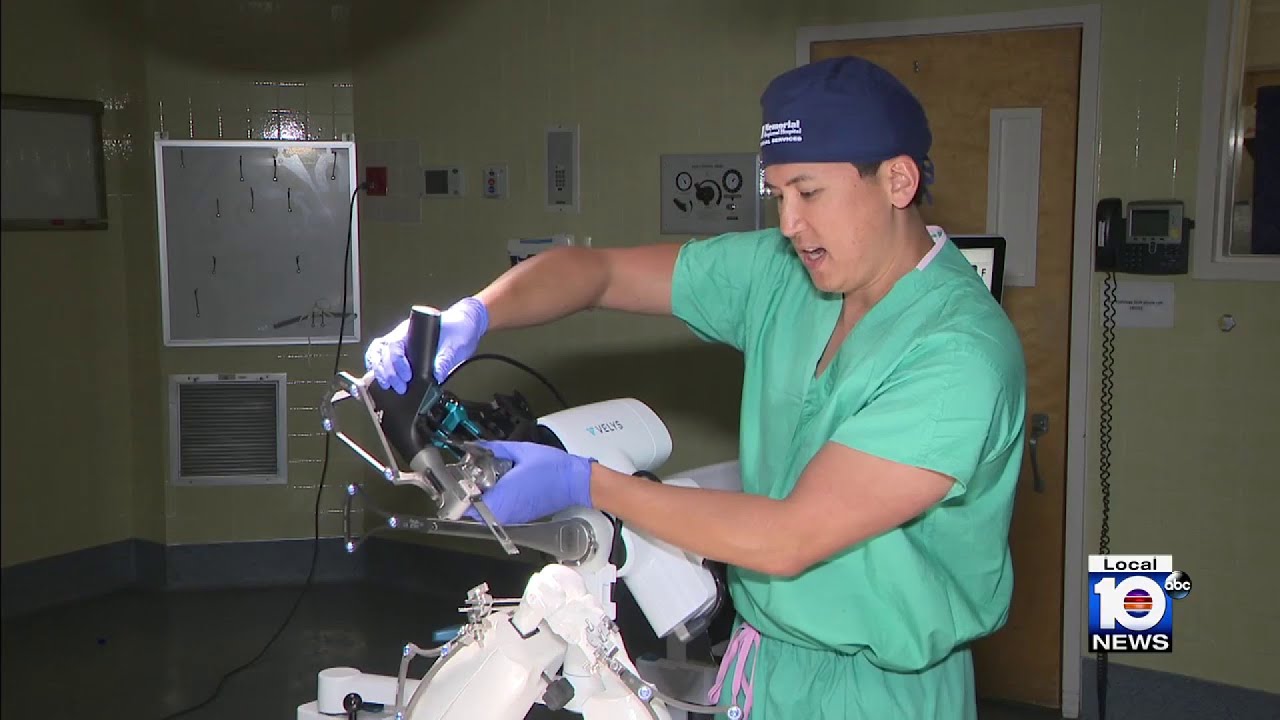
Dr. Ed Tingstad, Orthopedic Surgeon with Pullman Regional Hospital’s Orthopedic Center of Excellence and Inland Orthopaedic Surgery & Sports Medicine Clinic performs a total knee replacement using orthopedic robotics – VELYS. The VELYS Robotic-Assisted Solution technology makes for a more exact fitting knee replacement and uses intra-operative data to inform the surgeon during surgery. In this full-length total knee replacement video, Dr. Tingstad narrates a procedure from start to finish.
Learn more: pullmanregional.org/orthopedics

Eric knew he needed help when an old knee injury began worsening over the course of time and was significantly affecting his quality of life. That’s when he turned to his hometown orthopedic experts at Mayo Clinic Health System in Mankato, who recommended a total knee replacement. After overcoming some initial fears, Eric decided it was time to have the operation — a fuller and more active life with his family depended on it.

Carpal tunnel release (part 1). Skin incision and retraction. Procedure performed by Deepak Kapila, MD, Broward Health, Fort Lauderdale, FL. Courtesy of BroadcastMed (http://ortho.broadcastmed.com/....4229/videos/carpal-t
There are hundreds more procedural videos as well as news, features, resources and references on Medscape.com. Join today for free.

For a full Surgical Airway Techniques resource: https://bit.ly/2rb9Nud
Video courtesy of Gauri Mankekar, MBBS, MS, PhD

Join Dr. Parsia Vagefi, Chief of Surgical Transplantation and Dr. Steven Hanish, Surgical Director of Liver Transplantation, as they grant unprecedented access to the OR while performing a #Liver #Transplant #Surgery.
To find out more about UT Southwestern's transplant programs visit:
https://www.utswmed.org/transplant

Lattrell Wells was a perfect candidate for the MACI procedure. Dr. Michael O'Malley is a sports medicine surgeon at Carilion Clinic, "It’s a two stage procedure. So what we do is we actually harvest a small portion of the patient's cartilage and bone cells and we send it to a lab where the lab then that grows additional cartilage cells. It comes back to us in a little sheet and six weeks after that initial surgery, we re-implant the cartilage in a second surgery where we implant that sheet depending on the size of lesion right where his defect. This the only option where there’s virtually no risk of any kind of graft rejection or anything of that nature.

Lumpectomy means that a focal area of cancer is going to be removed. A lot of patients with a lumpectomy don’t need any specific breast reconstruction, explains Dr. Miguel Angel Medina, Director of Microsurgery with Miami Cancer Institute.
Al the end of surgical treatment, all those patients go on to need radiation therapy. For patients who have large breasts, physicians have to take a larger lumpectomy than normal.

How to perform a parotidectomy gland resection? In this video we take you step by step through the protid gland resection surgical technique. This video is intended for ENT residents and Head and Neck Surgery Surgeons. It is part of the ORL-Information's Head and Neck surgery Masterclass in collaboration with the University Hospital of Nîmes. Surgeons Editors: Pr. Benjamin LALLEMANT, MD, PhD - Dr. Camille GALY, MD Head and and Neck Department, University Hospital of Nîmes, France Official video | www.orl-information.fr
Cette vidéo présentent la technique de la parotidectomie avec dissection du nerf facial. Elle illustre les différents temps de l'intervention notamment le temps de repérage du nerf facial.
--------------------------------------
@Prévention médecine | Comment préserver sa santé ?
✔Abonnez-vous à la chaîne ORL-Information : https://www.youtube.com/c/ORLINFORMATION
✔Retrouvez-nous sur internet: https://www.orl-information.fr

Orthopedic spine surgeons and vascular surgeons at UW Health in Madison, WI work together to perform minimally invasive anterior lumbar interbody fusion (Mini-ALIF). With this type of spinal fusion surgery, patients have smaller incisions, usually spend less time in the hospital and typically return to daily activities more quickly. Learn more https://www.uwhealth.org/ALIF

A brain surgery called a craniectomy is performed to remove a part of your skull in order to relieve pressure in an area when your brain swells from a traumatic brain injury. It is also performed to treat medical conditions that cause your brain to swell or bleed that can be caused by an aneurysm, brain tumor or other cancer.
This 3d animation shows how the surgical procedure decreases intracranial pressure (ICP), intracranial hypertension (ICHT), or heavy bleeding (also called hemorrhaging) inside your skull. If left untreated, pressure or bleeding can compress your brain and push it down onto the brain stem. This can be fatal or cause permanent brain damage.
Brain surgery is a very serious procedure under any circumstances, but a craniectomy is done when there is an immediate risk to the brain and neurological function due to severe brain injury or stroke.
For more information about custom 3D animation depicting surgery, please visit https://www.amerra.com/.
Watch additional medical animations:
Accessing an implantable port training - 3D animation: https://youtu.be/xSTpxjyv4O4
Open Suctioning with a Tracheostomy Tube - 3D animation: https://youtu.be/wamB7jpWCiQ
Ventriculostomy Brain Surgery - 3d animation: https://youtu.be/pUy0YDzVNzs
Suctioning the endotracheal tube - medical animation: https://youtu.be/pN6-EYoeh3g
Functional endoscopic sinus surgery (FESS) - 3D animation: https://youtu.be/qKTRyowwaLA
How to insert a nasogastric tube for NG intubation - 3d animation: https://youtu.be/Abf3Gd6AaZQ
Oral airway insertion - oropharyngeal airway technique - 3D animation: https://youtu.be/caxUdNwjt34
Nasotracheal suctioning (NTS) - 3D animation: https://youtu.be/979jWMsF62c
Learn about hemorrhoids with #3d #animation: https://youtu.be/R6NqlMpsiiY
LASIK eye surgery - 3D animation: https://youtu.be/Bb8bnjnEM00
CPR cardiopulmonary resuscitation - 3D animation: https://youtu.be/G87knTZnhks
What are warts (HPV)? - 3D animation: https://youtu.be/guJ1J7rRs1w
How Macular Degeneration Affects Your Vision - 3D animation: https://youtu.be/ozZQIZ_52YY
NeoGraft hair transplant procedure – animation: https://youtu.be/C-eTdH2UPXI

Dr. Horacio Asbun, Mayo Clinic in Florida, explains the Whipple procedure using this animated graphic of a pancreas. Cancer of the pancreas affects 45,000 people every year in the U.S., and it is the fourth leading cause of cancer-related deaths. The five-year overall survival rate if a tumor is detected early and surgically removed is 22 percent, versus 6 percent without early detection and surgery. To learn more, visit http://mayocl.in/2zk7FDi.
This video in Spanish/español: https://www.youtube.com/watch?v=N_zWboNMKWk

Our mission: Empower you with the tools and support you need for weight loss and live a healthier life. Get started on your weight loss journey today: https://bit.ly/2Ms4JaX

For more information about Mohs surgery, please visit https://cle.clinic/3x7CRTy
Mohs surgery is a highly effective skin cancer removal procedure that takes just a few hours. It is most often used to treat basal cell and squamous cell carcinomas, the two most common skin cancers.
Chapters:
0:00 How effective is Mohs Surgery?
0:23 When is Mohs Surgery used?
0:50 How does Mohs Surgery work?
1:55 Does Mohs Surgery cure skin cancer?
2:06 How long is the recovery period after Mohs Surgery?
Resources:
Skins Cancer: https://cle.clinic/3G2MMM8
How Skin Cancer Is Found and Removed — At the Same Appointment: https://cle.clinic/3r9Wzu6
The Best Strategies To Reduce Your Risk of Skin Cancer: https://cle.clinic/38Bazqn
The information in this video was accurate as of 4.8.2022 and is for information purposes only. Consult your local medical authority or your healthcare practitioner for advice.
▶Share this video with others: https://youtu.be/aCV1UZ0Yj-o
▶Subscribe to learn more about Cleveland Clinic:
https://www.youtube.com/user/C....levelandClinic?sub_c
#ClevelandClinic #MohsSurgery #SkinCancer

It used to be when a woman needed a hysterectomy she could expect full abdominal surgery with a long recovery time. Dr. Melissa Lee uses less invasive methods that can cut the patients downtime in half.
"We were trained in more laparoscopic and minimally invasive cases so of course that's what I'm more comfortable with doing right now."
She sees a new generation of patients opting for laparoscopic surgery.
"Laparoscopy is the use of small cameras with small incisions and instruments that are guided by the hand, and you're able to see directly into the abdomen without actually fully opening the abdomen," says Dr. Lee, an obstetrician-gynecologist with Lee Memorial Health System.
Nowadays, even a large mass or uterus can be removed using the slender tools.
"There are multiple different laparoscopic instruments that you can use. Whether they're blunt dissections or just dissectors that hold and retract back or actual scissors or cutting instruments, there are multiple different options," says Dr. Lee.
While a standard abdominal hysterectomy requires a four to eight inch incision, the laparoscope needs only a quarter to half inch. It's enough to make a big difference in terms of recovery.
"They're able to get up and move around faster. They're able to recover faster, their pain level and their need for pain medicine is much lower," says Dr. Lee.
The laparoscopic procedure also cuts down on scarring and more importantly, shortens the hospital stay. The trend now is home within 24 hours.
"Where the patient is done early in the morning, they're doing well they're tolerating oral intake they're able to getup and move around. And those patients a lot of times will feel comfortable to go home that same nigh after a major surgery," says Dr. Lee.
New studies show women who've had a laparoscopic hysterectomy viewed their quality of life as better than those who had an open abdominal procedure, making this a good option for the right patient.
View More Health Matters video segments at leememorial.org/healthmatters/
Lee Memorial Health System in Fort Myers, FL is the largest network of medical care facilities in Southwest Florida and is highly respected for its expertise, innovation and quality of care. For nearly a century, we've been providing our community with everything from primary care treatment to highly specialized care services and robotic assisted surgeries.
Visit leememorial.org

.
Chapters
0:00 Introduction
1:04 Why do doctors perform laparoscopy?
2:11 How is laparoscopy performed?
3:22 Result
3:47 Risk of laparoscopy
Laparoscopy (from Ancient Greek λαπάρα (lapára) 'flank, side', and σκοπέω (skopéō) 'to see') is an operation performed in the abdomen or pelvis using small incisions (usually 0.5–1.5 cm) with the aid of a camera. The laparoscope aids diagnosis or therapeutic interventions with a few small cuts in the abdomen.[1]
Laparoscopic surgery, also called minimally invasive procedure, bandaid surgery, or keyhole surgery, is a modern surgical technique. There are a number of advantages to the patient with laparoscopic surgery versus an exploratory laparotomy. These include reduced pain due to smaller incisions, reduced hemorrhaging, and shorter recovery time. The key element is the use of a laparoscope, a long fiber optic cable system that allows viewing of the affected area by snaking the cable from a more distant, but more easily accessible location.
Laparoscopic surgery includes operations within the abdominal or pelvic cavities, whereas keyhole surgery performed on the thoracic or chest cavity is called thoracoscopic surgery. Specific surgical instruments used in laparoscopic surgery include obstetrical forceps, scissors, probes, dissectors, hooks, and retractors. Laparoscopic and thoracoscopic surgery belong to the broader field of endoscopy. The first laparoscopic procedure was performed by German surgeon Georg Kelling in 1901. There are two types of laparoscope:[2]
A telescopic rod lens system, usually connected to a video camera (single-chip or three-chip)
A digital laparoscope where a miniature digital video camera is placed at the end of the laparoscope, eliminating the rod lens system
The mechanism mentioned in the second type is mainly used to improve the image quality of flexible endoscopes, replacing conventional fiberscopes. Nevertheless, laparoscopes are rigid endoscopes. Rigidity is required in clinical practice. The rod-lens-based laparoscopes dominate overwhelmingly in practice, due to their fine optical resolution (50 µm typically, dependent on the aperture size used in the objective lens), and the image quality can be better than that of the digital camera if necessary. The second type of laparoscope is very rare in the laparoscope market and in hospitals.[citation needed]
Also attached is a fiber optic cable system connected to a "cold" light source (halogen or xenon) to illuminate the operative field, which is inserted through a 5 mm or 10 mm cannula or trocar. The abdomen is usually insufflated with carbon dioxide gas. This elevates the abdominal wall above the internal organs to create a working and viewing space. CO2 is used because it is common to the human body and can be absorbed by tissue and removed by the respiratory system. It is also non-flammable, which is important because electrosurgical devices are commonly used in laparoscopic procedures.[3]
Procedures
Surgeons perform laparoscopic stomach surgery.
Patient position
During the laparoscopic procedure, the position of the patient is either in Trendelenburg position or in reverse Trendelenburg. These positions have an effect on cardiopulmonary function. In Trendelenburg's position, there is an increased preload due to an increase in the venous return from lower extremities. This position results in cephalic shifting of the viscera, which accentuates the pressure on the diaphragm. In the case of reverse Trendelenburg position, pulmonary function tends to improve as there is a caudal shifting of viscera, which improves tidal volume by a decrease in the pressure on the diaphragm. This position also decreases the preload on the heart and causes a decrease in the venous return leading to hypotension. The pooling of blood in the lower extremities increases the stasis and predisposes the patient to develop deep vein thrombosis (DVT).[4]
Gallbladder
Rather than a minimum 20 cm incision as in traditional (open) cholecystectomy, four incisions of 0.5–1.0 cm, or more recently, a single incision of 1.5–2.0 cm,[5] will be sufficient to perform a laparoscopic removal of a gallbladder. Since the gallbladder is similar to a small balloon that stores and releases bile, it can usually be removed from the abdomen by suctioning out the bile and then removing the deflated gallbladder through the 1 cm incision at the patient's navel. The length of postoperative stay in the hospital is minimal, and same-day discharges are possible in cases of early morning procedures.[citation needed]
Colon and kidney

Dr. Celia Divino, Chief, Division of General Surgery at The Mount Sinai Hospital, performs a laparoscopic appendectomy. Visit the Division of General Surgery at http://bit.ly/18z944M. Click here to learn more about Dr. Celia Divino http://bit.ly/12RF0ee



