Top videos

The baby will move head down if there is room or if there is tone in the support to the uterus to direct baby head down. Before 24-26 weeks most babies lie diagonal or sideways in the Transverse Lie position. Between 24-29 weeks most babies turn vertical and some will be breech.

Watch more clips of Dr. James Kelly - https://www.youtube.com/playli....st?list=PLe2Je5-cHxP And for more information about brain injury and PTSD, please visit us at https://www.brainline.org.
Watch more clips of Pat LaFontaine - https://www.youtube.com/playli....st?list=PL5F3273C3C8
© 2018 WETA All Rights Reserved
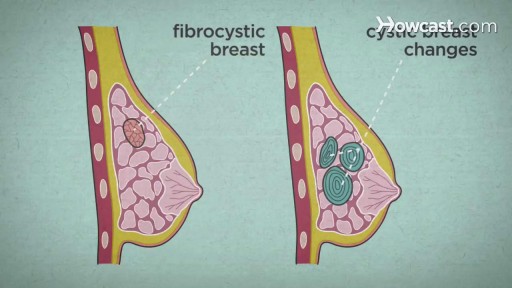
Over the course of a woman's lifetime, she may experience breast changes. While many end up being nothing to worry about, it's important to have any changes that you notice checked by a doctor -- just to be on the safe side. Here are the potential breast cancer symptoms to watch out for.

Ever heard medical terms like MRI or EKG? Funny speaker for nurses and doctors and all-around healthcare speaker Dr. Brad Nieder discusses the funny medical jargon he's encountered during his medical career.
He jokes about medical acronyms and big healthcare terms. His funny medical humor makes the conference attendees burst with laughter and he reads the medical definition for "laugh."
As an experienced physician and keynote speaker, he's perfect for any in-person or virtual conference or event. He's also a great healthcare speaker to bring in for continuing medical education (cme) units!
Learn more about Brad's keynote and virtual speaking, and book him for your next conference or virtual event: https://www.HealthyHumorist.com
Find Dr. Brad on social media:
https://www.facebook.com/HealthyHumor...
https://www.linkedin.com/in/BradNieder
https://twitter.com/HealthyHumorist
https://www.youtube.com/c/BradNiederMD
https://vimeo.com/BradNieder
Brad Nieder, MD, CSP*
The Healthy Humorist
Doctor, Keynote Speaker, Clean Comedian
*CSP=Certified Speaking Professional
"Medical Lingo"
From the DVD "The Healthy Humorist in Orlando: Laughter is the Best Medicine"

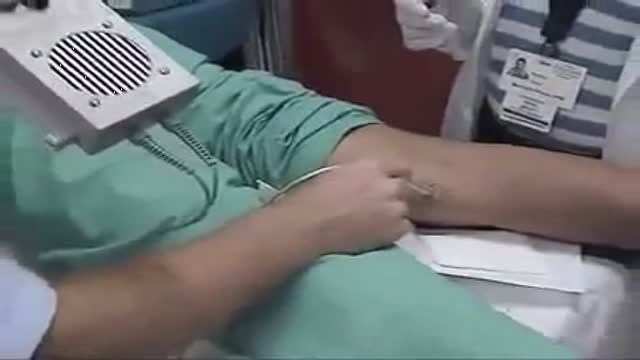
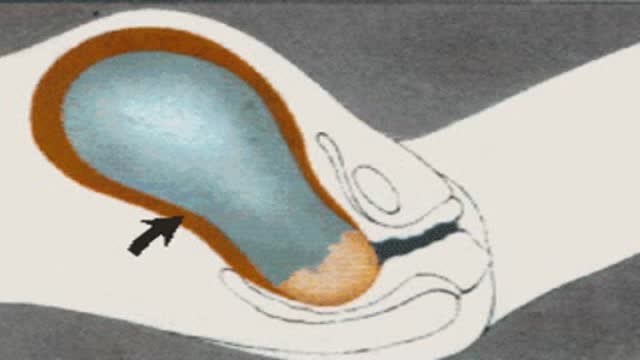
This video demonstrate Bilateral Salpingectomy for a patient suffering from hematosalpinx of one side and Hydrosalpinx other side in which one IVF has failed. Laparoscopic salpingectomy. In this less-invasive procedure, the surgeon makes 1-3 small incisions in the lower abdomen, and inserts a laparoscope into the pelvis through one of the incisions. The camera at the end of the laparoscope guides the surgeon through the procedure. The fallopian tube tissue is then removed. For more information https://www.laparoscopyhospital.com/
For more information please contact:
World Laparoscopy Hospital
Cyber City, Gurugram, NCR DELHI
INDIA 122002
Phone & WhatsApp: +919811416838, + 91 9999677788

Hirschsprung's (HIRSH-sproongz) disease is a condition that affects the large intestine (colon) and causes problems with passing stool. The condition is present at birth (congenital) as a result of missing nerve cells in the muscles of the baby's colon. A newborn who has Hirschsprung's disease usually can't have a bowel movement in the days after birth. In mild cases, the condition might not be detected until later in childhood. Uncommonly, Hirschsprung's disease is first diagnosed in adults.
Though the risk of HIV transmission through oral sex is very low, but several factors might increase the risk, including sores in the mouth or vagina or on the penis, bleeding gums, having an oral contact with menstrual blood, and the presence of other sexually transmitted diseases. But still the risk is low. by the way better to think twice before having the Oralsex with strangers. because you are not safe 100%.
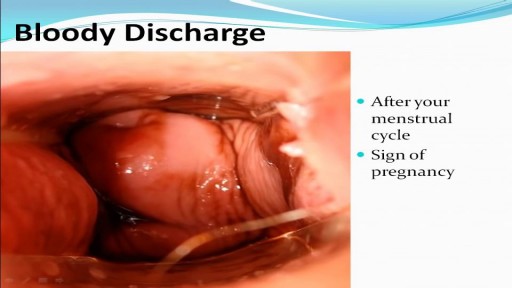
Childbirth (also called labour, birth, partus or parturition) is the culmination of a human pregnancy or gestation period with birth of one or more newborn infants from a woman’s uterus. The process of normal human childbirth is categorized in three stages of labour: the shortening and dilation of the cervix, descent and birth of the infant, and birth of the placenta. In some cases, childbirth is achieved through caesarean section, the removal of the neonate through a surgical incision in the abdomen, rather than through vaginal birth

https://www.O2Labz.com - Tummy tuck procedure animation.