Top videos

A plastic surgeon in China has successfully grown an artificial ear on a man's arm in a pioneering medical procedure. The patient, surnamed Ji, lost his right ear in an accident and yearned to have it back. Doctor Guo Shuzhong from a hospital in Xi'an, China's Shaanxi Province, used Mr Ji's cartilage from his ribs to build the new ear; and he expects to transplanted the organ to the man's head in about four months. According to the Huanqiu report, Mr Ji sustained serious injuries in the right side of his face in a traffic accident about a year ago. His right ear was torn from his face. The man, whose age is not specified, has since received multiple surgical operations to restore his facial skin and his cheeks. However, he felt frustrated about losing his right ear for good. The patient told a report from China News: 'I lost one ear. I have always felt that I am not complete.' Having sought medical advice from multiple sources, Ji realised that it was impossible to restore his ear through conventional medical procedures as a substantial part of his right ear had gone missing. Upon hearing recommendations, Mr Ji went to see doctor Guo Shuzhong, who works at the First Affiliated Hospital of Xi'an Jiaotong University in the city of Xi'an. Doctor Guo, a renowned plastic surgeon, conducted China's first face transplant operation in 2006, according to China Daily.
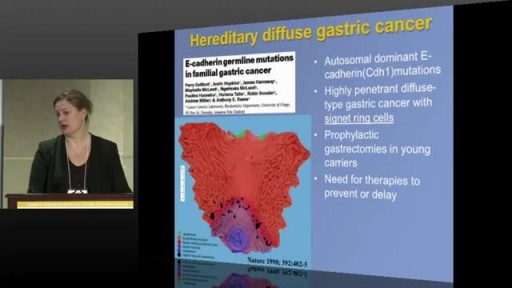
Stomach cancer usually begins in the mucus-producing cells that line the stomach. This type of cancer is called adenocarcinoma. For the past several decades, rates of cancer in the main part of the stomach (stomach body) have been falling worldwide. During the same period, cancer in the area where the top part of the stomach (cardia) meets the lower end of the swallowing tube (esophagus) has become much more common. This area of the stomach is called the gastroesophageal junction.

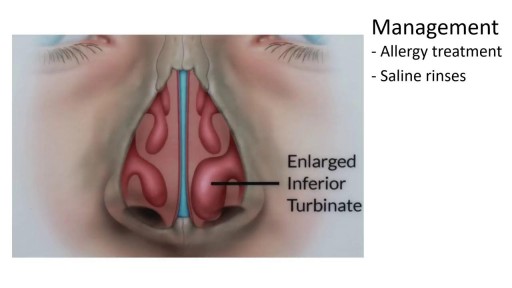
Causes are chronic inflammation due to infection, allergies, drug sensitivity, or immune disorders. Symptoms may include a runny nose, stuffiness, or post-nasal drip. In some cases, there may be no symptoms. The condition can be treated with corticosteroids, other medications, or surgery.

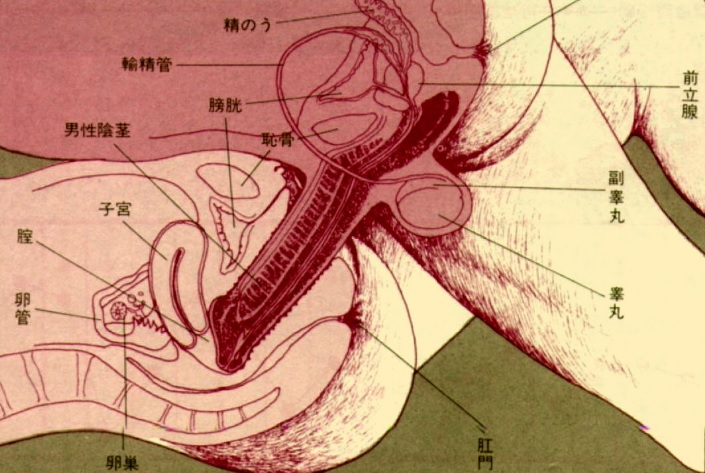
Sexually Transmitted Diseases (STDs) affect millions of people each year. The most common STDs are gonorrhea, chlamydia and trichomoniasis. While even thinking about STDs and whether you may have one is scary, knowing the facts can make a big difference in your long-term health. Here is what you need to know:
People who are sexually active with multiple partners and are not using barrier protection are at most risk. Teenagers are a large part of this group, because they dont always practice safe sex and they are more likely to have multiple partners. It is recommended that women who are sexually active with multiple partners get screened yearly or immediately after they have engaged in unprotected sex. If you discover that you have an STD, both you and your partner would most likely be treated with antibiotics.
Gonorrhea
Approximately 350,000 cases of gonorrhea were reported to the CDC in 2006, but because not everyone is getting tested for STDs, experts believe the actual numbers are twice that.
The symptoms for gonorrhea are burning with urination, abnormal discharge or pelvic pain. Pelvic pain indicates a very severe infection. Untreated gonorrhea can lead to a serious infection as the disease may spread to a womans fallopian tubes and cause infertility.
Chlamydia
There were 1,000,000 cases of chlamydia reported to the CDC in 2006; experts think the actual rate of infection is as high as 2,000,000 cases.
Chlamydia is often called the silent disease because many people with chlamydia have no symptoms. Chlamydia can affect the urethra, the vagina, the cervix and the fallopian tubes. Symptoms include burring with urination, abnormal discharge and pelvic pain. If you are experiencing any of these systems you should see your doctor to determine if you have chlamydia. Women with chlamydia who arent treated are likely to develop pelvic inflammatory disease. Pelvic inflammatory disease occurs when the infection spreads and causes scarring to the uterus and fallopian tubes. Untreated chlamydia can result in infertility.
Trichomoniasis
Trichomoniasis is the most common STD. About 7 million women and men have trichomoniasis. Women who have trichomoniasis will often experience a frothy yellow or green discharge coming from their vagina. But some people wont have any symptoms.
Understanding STDs, what causes them, and how to treat them will help you stay in control of your health.

Wisdom teeth extractions can rear their ugly head later in life. This is a video of a patient with neck pain and neck weakness. When we stimulated the nerve fibers in the area of the extracted teeth there was an immediate improvement in her ability to control her neck muscles.

Site enhancement oil, often called "santol" or "synthol" (no relation to the Synthol mouthwash brand), refers to oils injected into muscles to increase the size or change the shape. Some bodybuilders, particularly at the professional level, inject their muscles with such mixtures to mimic the appearance of developed muscle where it may otherwise be disproportionate or lagging. This is known as "fluffing".Synthol is 85% oil, 7.5% lidocaine, and 7.5% alcohol. It is not restricted, and many brands are available on the Internet. The use of injected oil to enhance muscle appearance is common among bodybuilders, despite the fact that synthol can cause pulmonary embolisms, nerve damage, infections, sclerosing lipogranuloma,[60] stroke,[55] and the formation of oil-filled granulomas, cysts or ulcers in the muscle. Rare cases might require surgical intervention to avoid further damage to the muscle and/or to prevent loss of life. Sesame oil is often used in such mixtures, which can cause allergic reactions such as vasculitis.
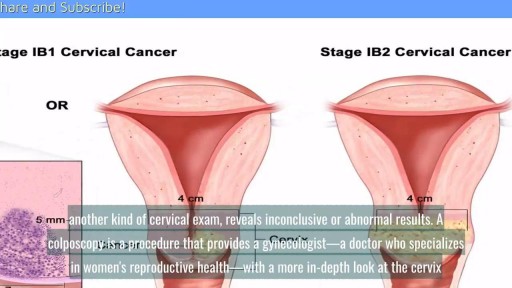
A cervical biopsy is a procedure that is sometimes done on women during an exam called a colposcopy to remove cervical tissue for examination. It is also called a punch biopsy. It is usually performed when a Pap smear result is either inconclusive or abnormal and a doctor wants to screen further for any cervical dysplasia or cervical cancer.
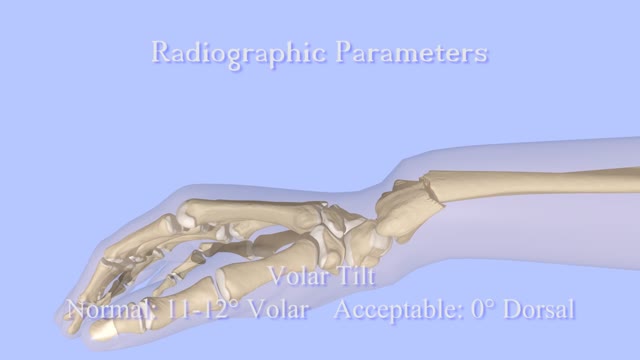
Closed Reduction of Distal Radius Fractures - Discussion: (distal radius fracture menu) - closed reduction & immobilization in plaster cast remains accepted method of treatment for majority of stable distal radius frx; - unstable fractures will often lose reduction in the cast and will slip back to the pre-reduction position; - patients should be examined for carpal tunnel symptoms before and after reduction; - carpal tunnel symptoms that do not resolve following reduction will require carpal tunnel release; - cautions: - The efficacy of closed reduction in displaced distal radius fractures. - Technique: - anesthesia: (see: anesthesia menu) - hematoma block w/ lidocaine; - w/ hematoma block surgeon should look for "flash back" of blood from hematoma, prior to injection; - references: - Regional anesthesia preferable for Colles' fracture. Controlled comparison with local anesthesia. - Neurological complications of dynamic reduction of Colles' fractures without anesthesia compared with traditional manipulation after local infiltration anesthesia. - methods of reduction: - Jones method: involves increasing deformity, applying traction, and immobilizing hand & wrist in reduced position; - placing hand & wrist in too much flexion (Cotton-Loder position) leads to median nerve compression & stiff fingers; - Bohler advocated longitudinal traction followed by extension and realignment; - consider hyper-extending the distal fragment, and then translating it distally (while in extended position) until it can be "hooked over" proximal fragment; - subsequently, the distal fragment can be flexed (or hinged) over the proximal shaft fragment; - closed reduction of distal radius fractures is facilitated by having an assistant provide counter traction (above the elbow) while the surgeon controls the distal fragment w/ both hands (both thumbs over the dorsal surface of the distal fragment); - flouroscopy: - it allows a quick, gentle, and complete reduction; - prepare are by prewrapping the arm w/ sheet cotton and have the plaster or fibroglass ready; - if flouroscopy is not available, then do not pre-wrap the extremity w/ cotton; - it will be necessary to palpate the landmarks (outer shaped of radius, radial styloid, and Lister's tubercle, in order to judge success of reduction; - casting: - generally, the surgeon will use a pre-measured double sugar sugar tong splint, which is 6-8 layers in thickness; - more than 8 layers of plaster can cause full thickness burns: - reference: Setting temperatures of synthetic casts. - position of immobilization - follow up: - radiographs: - repeat radiographs are required weekly for 2-3 weeks to ensure that there is maintenance of the reduction; - a fracture reduction that slips should be considered to be unstable and probably require fixation with (pins, or ex fix ect.) - there is some evidence that remanipulation following fracture displacement in cast is not effective for these fractures; - ultimately, whether or not a patient is satisfied with the results of non operative treatment depends heavily on th
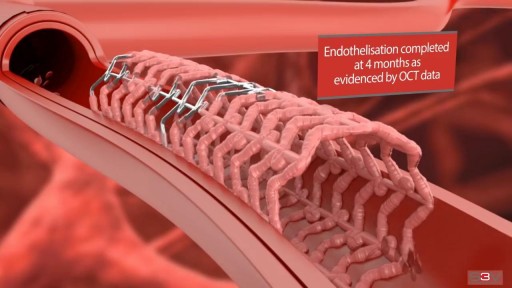
Angioplasty is a procedure to restore blood flow through the artery. You have angioplasty in a hospital. The doctor threads a thin tube through a blood vessel in the arm or groin up to the involved site in the artery. The tube has a tiny balloon on the end.

Preeclampsia is a pregnancy complication characterized by high blood pressure and signs of damage to another organ system, often the kidneys. Preeclampsia usually begins after 20 weeks of pregnancy in a woman whose blood pressure had been normal. Even a slight rise in blood pressure may be a sign of preeclampsia. Left untreated, preeclampsia can lead to serious — even fatal — complications for both you and your baby. If you have preeclampsia, the only cure is delivery of your baby. If you're diagnosed with preeclampsia too early in your pregnancy to deliver your baby, you and your doctor face a challenging task. Your baby needs more time to mature, but you need to avoid putting yourself or your baby at risk of serious complications.