Top videos

The Ortolani method is an examination method that identifies a dislocated hip that can be reduced into the socket (acetabulum). Ortolani described the feeling of reduction as a “Hip Click” but the translation from Italian was interpreted a sound instead of a sensation of the hip moving over the edge of the socket when it re-located. After the age of six weeks, this sensation is rarely detectable and should not be confused with snapping that is common and can occur in stable hips when ligaments in and around the hip create clicking noises. When the Ortolani test is positive because the hip is dislocated, treatment is recommended to keep the hip in the socket until stability has been established

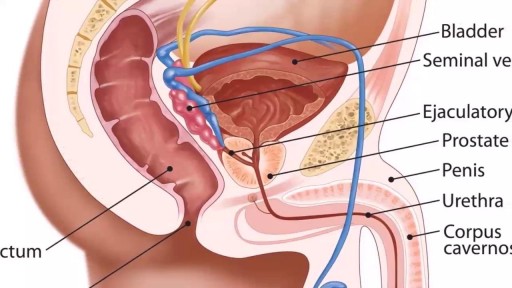
Cystoscopy (sis-TOS-kuh-pee) is a procedure that allows your doctor to examine the lining of your bladder and the tube that carries urine out of your body (urethra). A hollow tube (cystoscope) equipped with a lens is inserted into your urethra and slowly advanced into your bladder.

This video provides a demonstration of how to assess for transillumination when assessing scrotal swelling.
Read our step-by-step guide here: https://geekymedics.com/testic....ular-examination-osc
Check out our other awesome clinical skills resources, including:
• 🔥 Geeky Medics Bundles (discounted products): https://app.geekymedics.com/purchase/bundles/
• ✨ 1000+ OSCE Stations: https://app.geekymedics.com/pu....rchase/osce-stations
• 🏥 Geeky Medics OSCE Revision Book: https://app.geekymedics.com/purchase/book/
• 📝 150+ PDF OSCE Checklists: https://geekymedics.com/pdf-osce-checklists/
• 🗂️ 3000+ OSCE Flashcards: https://app.geekymedics.com/pu....rchase/flashcard-col
• 📱 Geeky Medics OSCE App: https://geekymedics.com/geeky-medics-app/
• 🩺 Medical Finals SBA Question Pack: https://app.geekymedics.com/pu....rchase/medical-stude
• 💊 PSA Question Pack: https://app.geekymedics.com/pu....rchase/prescribing-s
Subscribe to our newsletter to be the first to know about our latest content: https://geekymedics.com/newsletter/ ✉️
Join the Geeky Medics community: 👩👩👧👧
Twitter: http://www.twitter.com/geekymedics
Instagram: https://instagram.com/geekymedics
Facebook: http://www.facebook.com/geekymedics
Always adhere to your medical school/local hospital guidelines when performing examinations or clinical procedures. DO NOT perform any examination or procedure on patients based purely on the content of these videos. Geeky Medics accepts no liability for loss of any kind incurred as a result of reliance upon the information provided in this video.
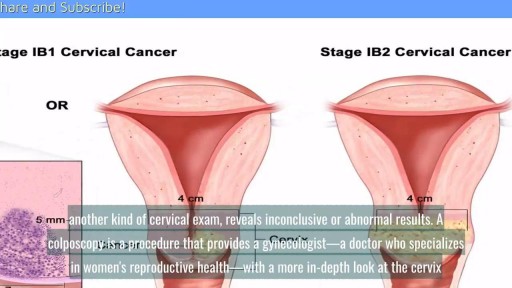
A cervical biopsy is a procedure that is sometimes done on women during an exam called a colposcopy to remove cervical tissue for examination. It is also called a punch biopsy. It is usually performed when a Pap smear result is either inconclusive or abnormal and a doctor wants to screen further for any cervical dysplasia or cervical cancer.

Urinary incontinence isn't a disease, it's a symptom. It can be caused by everyday habits, underlying medical conditions or physical problems. A thorough evaluation by your doctor can help determine what's behind your incontinence. Temporary urinary incontinence Certain drinks, foods and medications can act as diuretics — stimulating your bladder and increasing your volume of urine. They include: Alcohol Caffeine Decaffeinated tea and coffee Carbonated drinks Artificial sweeteners Corn syrup Foods that are high in spice, sugar or acid, especially citrus fruits Heart and blood pressure medications, sedatives, and muscle relaxants Large doses of vitamins B or C Urinary incontinence also may be caused by an easily treatable medical condition, such as: Urinary tract infection. Infections can irritate your bladder, causing you to have strong urges to urinate, and sometimes incontinence. Other signs and symptoms of urinary tract infection include a burning sensation when you urinate and foul-smelling urine. Constipation. The rectum is located near the bladder and shares many of the same nerves. Hard, compacted stool in your rectum causes these nerves to be overactive and increase urinary frequency. Persistent urinary incontinence Urinary incontinence can also be a persistent condition caused by underlying physical problems or changes, including: Pregnancy. Hormonal changes and the increased weight of the uterus can lead to stress incontinence. Childbirth. Vaginal delivery can weaken muscles needed for bladder control and also damage bladder nerves and supportive tissue, leading to a dropped (prolapsed) pelvic floor. With prolapse, the bladder, uterus, rectum or small intestine can get pushed down from the usual position and protrude into the vagina. Such protrusions can be associated with incontinence. Changes with age. Aging of the bladder muscle can decrease the bladder's capacity to store urine. Menopause. After menopause women produce less estrogen, a hormone that helps keep the lining of the bladder and urethra healthy. Deterioration of these tissues can aggravate incontinence. Hysterectomy. In women, the bladder and uterus are supported by many of the same muscles and ligaments. Any surgery that involves a woman's reproductive system, including removal of the uterus, may damage the supporting pelvic floor muscles, which can lead to incontinence. Enlarged prostate. Especially in older men, incontinence often stems from enlargement of the prostate gland, a condition known as benign prostatic hyperplasia. Prostate cancer. In men, stress incontinence or urge incontinence can be associated with untreated prostate cancer. But more often, incontinence is a side effect of treatments for prostate cancer. Obstruction. A tumor anywhere along your urinary tract can block the normal flow of urine, leading to overflow incontinence. Urinary stones — hard, stone-like masses that form in the bladder — sometimes cause urine leakage. Neurological disorders. Multiple sclerosis, Parkinson's disease, stroke, a brain tumor or a spinal injury can interfere with nerve signals involved in bladder control, causing urinary incontinence.

Colonoscopy is a test that allows your doctor to look at the inner lining of your large intestine (rectum and colon). He or she uses a thin, flexible tube called a colonoscope to look at the colon. A colonoscopy helps find ulcers, colon polyps, tumors, and areas of inflammation or bleeding.

This video has been updated to include an alternate name for the internal thoracic arteries. View the updated video here: https://youtu.be/kxc22Fjd1NQ
For Employees of Hospitals, Schools, Universities and Libraries: Download 8 FREE medical animations from Nucleus by signing up for a free trial: http://nmal.nucleusmedicalmedi....a.com/free-trial-mem
Biology students: Subscribe to the Nucleus Biology channel to see new animations on biology and other science topics, plus short quizzes to ace your next exam: https://bit.ly/3lH1CzV
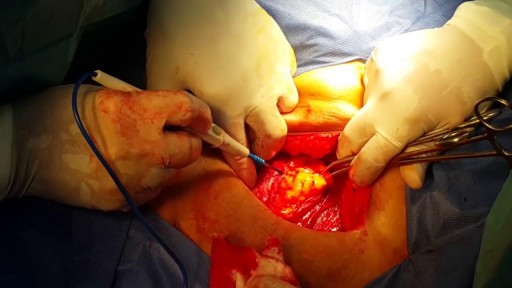
This video, created by Nucleus Medical Media, shows a coronary artery bypass graft (CABG) procedure used to combat coronary artery disease. Beginning with a midline sternal incision, the heart is connected to a perfusion machine which will take over the duties of the heart while the surgery takes place. Two different grafts are used to bypass the blocked coronary arteries: the internal thoracic artery from inside the chest wall, and the saphenous vein from the leg. After the procedure, the heart is shocked to restart its beating. A drainage tube is left at the incision site to drain away excess fluid. The animation continues to show two other types of approaches to a coronary artery bypass graft, off-pump bypass surgery and minimally invasive bypass surgery.
This is similar to the procedure performed on former president Bill Clinton and former California governor Arnold Schwarzenegger.
#HeartBypassSurgery #CABG #heart
ANCE00199

This patient presented to the ER for umbilical pain and had a history of umbilical hernia. He was concerned about the possibility of incarceration of the hernia.
In this video we explain how the clinical exam helps to differentiate a simple painful hernia from an incarcerated one.
***Thanks to the patient for sharing his history and exam with YouTube world***

The examination room should be quiet, warm and well lit. After you have finished interviewing the patient, provide them with a gown (a.k.a. "Johnny") and leave the room (or draw a separating curtain) while they change. Instruct them to remove all of their clothing (except for briefs) and put on the gown so that the opening is in the rear. Occasionally, patient's will end up using them as ponchos, capes or in other creative ways. While this may make for a more attractive ensemble it will also, unfortunately, interfere with your ability to perform an examination! Prior to measuring vital signs, the patient should have had the opportunity to sit for approximately five minutes so that the values are not affected by the exertion required to walk to the exam room. All measurements are made while the patient is seated. Observation: Before diving in, take a minute or so to look at the patient in their entirety, making your observations, if possible, from an out-of-the way perch. Does the patient seem anxious, in pain, upset? What about their dress and hygiene? Remember, the exam begins as soon as you lay eyes on the patient. Temperature: This is generally obtained using an oral thermometer that provides a digital reading when the sensor is placed under the patient's tongue. As most exam rooms do not have thermometers, it is not necessary to repeat this measurement unless, of course, the recorded value seems discordant with the patient's clinical condition (e.g. they feel hot but reportedly have no fever or vice versa). Depending on the bias of a particular institution, temperature is measured in either Celcius or Farenheit, with a fever defined as greater than 38-38.5 C or 101-101.5 F. Rectal temperatures, which most closely reflect internal or core values, are approximately 1 degree F higher than those obtained orally. Respiratory Rate: Respirations are recorded as breaths per minute. They should be counted for at least 30 seconds as the total number of breaths in a 15 second period is rather small and any miscounting can result in rather large errors when multiplied by 4. Try to do this as surreptitiously as possible so that the patient does not consciously alter their rate of breathing. This can be done by observing the rise and fall of the patient's hospital gown while you appear to be taking their pulse. Normal is between 12 and 20. In general, this measurement offers no relevant information for the routine examination. However, particularly in the setting of cardio-pulmonary illness, it can be a very reliable marker of disease activity. Pulse: This can be measured at any place where there is a large artery (e.g. carotid, femoral, or simply by listening over the heart), though for the sake of convenience it is generally done by palpating the radial impulse. You may find it helpful to feel both radial arteries simultaneously, doubling the sensory input and helping to insure the accuracy of your measurements. Place the tips of your index and middle fingers just proximal to the patients wrist on the thumb side, orienting them so that they are both over the length of the vessel.