Top videos
The cervix is fully dilated to about 10 cm,with the baby's head moving beyond the cervical opening , into the birth canal. The mother is encouraged to push during contractions,and rest in between them. In a normal delivery, the head rotates to face the mother's back
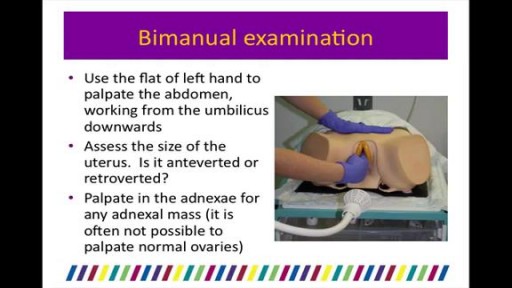
During the examination, the doctor gently puts a lubricated, gloved finger of one hand into the rectum. He or she may use the other hand to press on the lower belly or pelvic area. A digital rectal exam is done for men as part of a complete physical examination to check the prostate gland .

http://drraewynteirney.com.au/video/
http://drraewynteirney.com.au/....about-dr-raewyn-teir
Dr Raewyn Teirney - fertility specialist and Gynaecologist in Sydney shows a video recording of a laparoscopy for a woman with infertility and pelvic pain.
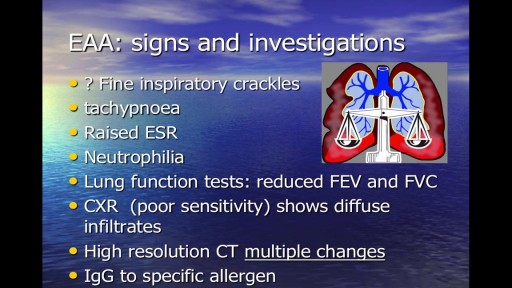
Occupational respiratory disease is any lung condition you get at work. Certain workplaces lend themselves to disease. The most common are coalmines and factories or areas with high amounts of toxins. These include asbestos and silica dust, as well as smoke, fumes, gases, and other particles. Types of occupational respiratory disease include: coal workers’ pneumoconiosis, also known as Black Lung Disease asbestosis silicosis farmers’ lung, also known as allergic alveolitis. It also includes forms of asthma, bronchitis, or emphysema.
An undescended testicle (cryptorchidism) is a testicle that hasn't moved into its proper position in the bag of skin hanging below the penis (scrotum) before birth. Usually just one testicle is affected, but about 10 percent of the time both testicles are undescended. An undescended testicle is uncommon in general, but common among baby boys born prematurely. The vast majority of the time, the undescended testicle moves into the proper position on its own, within the first few months of life. If your son has an undescended testicle that doesn't correct itself, surgery can relocate the testicle into the scrotum.

Alexandra J. Golby, MD, Director, Image-guided Neurosurgery at Brigham and Women’s Hospital, discusses technological advancements to improve the precision of surgery to remove brain tumors.
It’s estimated that each year nearly 80,000 people are diagnosed with primary brain tumors and 100,000 with metastatic brain tumors. Nearly everybody is at risk for developing a brain tumor. Brain tumors can affect people from childhood to the last years of their lives. Men are slightly more affected than women and the causes of most brain tumors are not known.
There are a number of unique challenges in treating brain tumors. One challenge is that primary tumors can have indistinct margins that are difficult to see. Another challenge is that the tissue around a brain tumor is uniquely important and may impact things like language, visual and motor function.
The AMIGO Suite, opened in 2011 at Brigham and Women’s Hospital, is the Advanced Multimodality Image Guided Operating Suite. It's an NIH-funded national center which was developed with the goal of translating technological advances into improvements in surgical and interventional care for patients. In the AMIGO Suite, there is an intraoperative MRI scanner which can be brought in and out of the operating room during surgery to help surgeons visualize a patient’s tumor better.
Image-guided surgery uses the information obtained from advanced imaging and translates that into the planning and execution of surgery by acquiring high resolution and specialty structural images of the brain and also functional images of the brain. These images can be registered to one another and then to the patient's head during surgery. This allows surgeons to pinpoint the location of the tumor as well as the areas that we would like to preserve, areas that serve critical brain functions are located.
One of the big challenges, even with image-guided surgery, is that as we perform the surgery, the configuration of the brain is changing, and we call that brain shift. And it's due to changes in the brain itself and also as we remove tissue, things are constantly shifting and moving. When we're talking about doing brain tumor surgery, a few millimeters of movement can be a big difference. How to measure and track brain shift is an important area of research and a number of technologies are being studied to understand how to measure brain shift during surgery.
The development of various intraoperative imaging technologies allows surgeons to provide the most accurate surgical treatment for each individual patient.
Learn more about precision brain surgery at Brigham and Women’s Hospital:
https://www.brighamandwomens.o....rg/neurosurgery/brai
There many concerns and questions about how a breast augmentation procedure works. Dr. Linder a highly qualified plastic surgeon based in Beverly Hills, demystifies those worries. Dr. Stuart Linder is a Beverly Hills board certified plastic surgeon, specializing in body sculpting and reconstructive procedures including breast augmentation, reduction, lift, liposuction and tummy tuck. He is board-certified by the American Board of Plastic Surgery and is affiliated with the American College of Surgeons, the American Society of Plastic and Reconstructive Surgeons and the American Medical Association. Website: www.drlinder.com
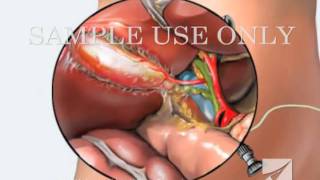
This medical animation shows laparoscopically assisted gallbladder removal surgery, or cholecystectomy. The animation begins by showing the normal anatomy of the liver and gallbladder. Over time, gallstones form within the gallbladder, blocking the cystic duct, and causing the gallbladder to become enlarged and inflamed. The procedure, sometimes called a "lap-chole", begins with the insertion of four trocar devices, which allow the physician to see inside the abdomen without making a large incision. Air is added to the abdominal cavity to make it easier to see the gall bladder. Next, we see a view through the laparascope, showing two surgical instruments grasping the gallbladder while a third severs the cystic duct. After the gallbladder is removed, the camera pans around to show that the cystic artery and vein, have already been clipped to prevent bleeding.
Item #ANIM026

Since the first replant more than 50 years ago, thousands of severed body parts have been reattached, preserving the quality of life for thousands of patients through improved function and appearance that the void remaining after amputation cannot provide. Ronald Malt performed the first replantation on May 23, 1962 at Massachusetts General Hospital on a 12-year-old boy who had his right arm amputated in a train accident. [1, 2] This amputation occurred at the level of the humeral neck.