Top videos

This poor old lady came with swelling in her left buttock for 10 days.She had history of injection in her buttocks two weeks back. She developed painful swelling and redness in her left gluteal region with difficulty in walking.It was diagnosed as injection abscess left gluteal region which needs incision and drainage under local anesthesia.Patient part painted and drapped.2% Lignocaine with adrenaline was infiltrated around the swelling for proper filed block.I use no-11 blade for stab incision over the swelling at the most fluctuating point of the abscess.You can watch how pus was flowing out from the cavity.The aim is to drain all pus from the abscess cavity.Finger exploration is essential to break all loculi inside the cavity, to know the depth and extend of the cavity and to fascilitate proper drainage of residual pus.after pus evacuation,, the cavity should be irrigated with normal saline and betadine solution.lastly the cavity to be packed with betadine soaked guage pieces.Proper dressing is essential.the dressing to be changed after 24 hours.daily dressing is essential with a good antibiotic coverage.the cavity usually obliterates within a period of seven to ten days.

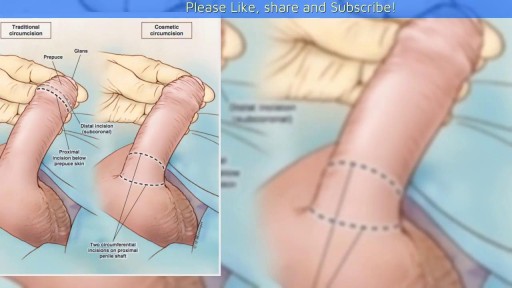
Female Circumcision - FGM Female Genital Mutilation - female circumcision ختان الاناث - женское обрезание - circuncisão feminina - 女性割禮 - besnijdenis - babae pagtutuli - l'excision - κλειτοριδεκτομή - הנקבה מולה - sunat perempuan - circoncisione femminile - 女子割礼 - 여성 할례 - la circuncisión femenina - หญิง circumcision - kadın sünnet - жіноче обрізання For More read at World Health Organization web site : http://www.who.int/topics/female_genital_mutilation/en/index.html other sites : http://en.wikipedia.org/wiki/Female_genital_cutting
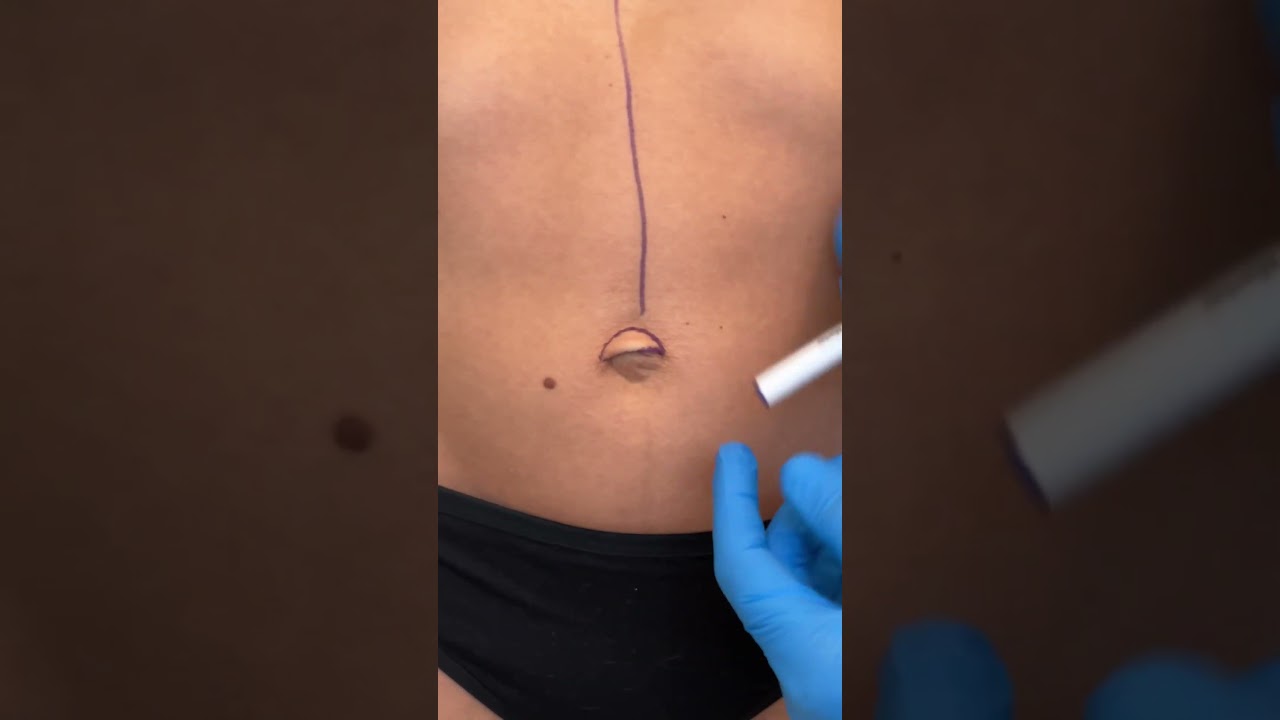
Check out @barrettplasticsurgery on TikTok!
Like and subscribe for more! #shorts #medical #plasticsurgery
More information:
www.drdanielbarrett.com
![Female Foley Insertion (Urinary Catheter) [How to Insert Nursing Skills]](https://i.ytimg.com/vi/Mq4Yh0-iozY/maxresdefault.jpg)
Pass your tests and improve your grades with the below FREE resources:
1) A FREE 140 Must Know Meds book
Click here to get your FREE copy of the 140 Must Know Meds Book: https://bit.ly/41rxSt0
2) A FREE test-taking tips webinar
Join us for our free test-taking tips webinar to boost your exam scores: https://bit.ly/nursingtesttaking
You can now test your knowledge with a free lesson quiz on NURSING.com!
Click here to take a free quiz: https://bit.ly/3HwJr8t
FREE Nursing School Cheat Sheets at: http://www.NURSING.com
Get the full lesson on Female Foley Insertion here:
https://nursing.com/lesson/ski....lls-03-01-inserting-
Get the Male Foley Insertion lesson here:
https://nursing.com/lesson/ski....lls-03-02-inserting-
Get the Sterile glove application lesson here:
https://nursing.com/lesson/ski....lls-01-04-sterile-gl
Check out our new Nurse Care Plan Lessons here:
https://bit.ly/3BPRfPL
Get Access to Thousands of Lessons here:
https://nursing.com/courses/
Welcome to the NURSING Family, we call it the most supportive nursing cohort on the planet.
At NURSING.com, we want to help you remove the stress and overwhelm of nursing school so that you can focus on becoming an amazing nurse.
Check out our freebies and learn more at: (http://www.nursing.com)
Female Foley Insertion (Urinary Catheter)- Nursing Skills
In this video, we’re going to look at inserting a Foley catheter in a female. Of course make sure you’ve verified your order and told the patient what’s happening. You’ll also typically want to perform perineal care before you start. Then, you’ll want to assist the patient into the appropriate position. For females, that’s supine with their knees bent and feet close to their hips – allowing their knees to fall to the side. You may need a helper to help hold the patient in this position. We love you guys! Go out and be your best selves today! And, as always, happy nursing!
Bookmarks:
0.05 Female Foley insertion introduction
0.15 Patient positioning
0.27 Opening the sterile kit
1.41 Setting up the sterile field
2.25 Prepping the remaining Foley kit items
2.34 Catheter lubrication
3.00 Saline syringe attachment
3.10 Iodine, swabs and cleansing the area
3.52 Catheter insertion (into urethra)
4.06 Balloon inflation
4.25 Final catheter setting
4.31 Securing the catheter and bag
4.48 Discarding your supplies
5.00 Documentation
5.08 Foley insertion outro
Visit us at https://nursing.com/medical-disclaimer/ for disclaimer information.
NCLEX®, NCLEX-RN® are registered trademarks of the National Council of State Boards of Nursing, INC. and hold no affiliation with NURSING.com.

-The cremasteric reflex test is considered positive if there is elevation of the testis in response to stroking the upper inner thigh. This reaction is typically absent in testicular torsion and boys under the age of 6 months. Although not completely reliable in older boys and adults, an absent cremasteric reflex is highly suggestive of torsion. Patients with epididymitis usually have a normal cremasteric reflex, with pain and swelling isolated to

Colonoscopy is a test that allows your doctor to look at the inner lining of your large intestine (rectum and colon). He or she uses a thin, flexible tube called a colonoscope to look at the colon. A colonoscopy helps find ulcers, colon polyps, tumors, and areas of inflammation or bleeding.

http://drraewynteirney.com.au/video/
http://drraewynteirney.com.au/....about-dr-raewyn-teir
Dr Raewyn Teirney - fertility specialist and Gynaecologist in Sydney shows a video recording of a laparoscopy for a woman with infertility and pelvic pain.