Top videos

From our beginnings in 1990 in primary healthcare, Healthway Medical has grown to become a respected medical group in Singapore. With over 100 clinics and medical centres, Healthway Medical has a wide network of medical centres and clinics in Singapore.
We offer comprehensive services including GP & family medicine clinics, health screening, adult specialists, baby & child specialists, dental services and allied healthcare services.
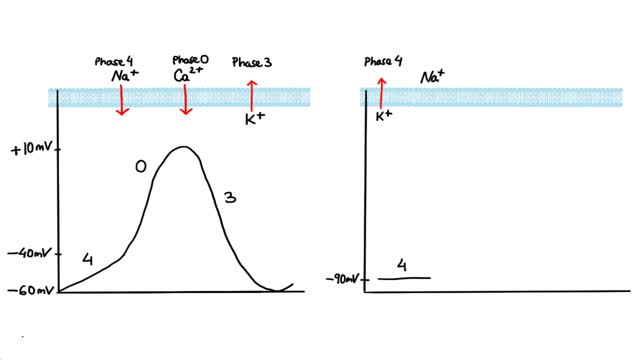
Antiarrhythmics are drugs that are used to treat abnormal heart rhythms resulting from irregular electrical activity of the heart. There are many different types of antiarrhythmic drugs. Examples include: Amiodarone (Cordarone) Flecainide (Tambocor) Procainamide (Procanbid) Sotalol (Betapace) In addition, there are other types of heart drugs that can be used to treat arrhythmias, including: Beta-blockers such as metoprolol or Toprol XL, which reduce the heart's workload and heart rate. Calcium channel blockers such as verapamil or Calan, which also reduces the heart rate.
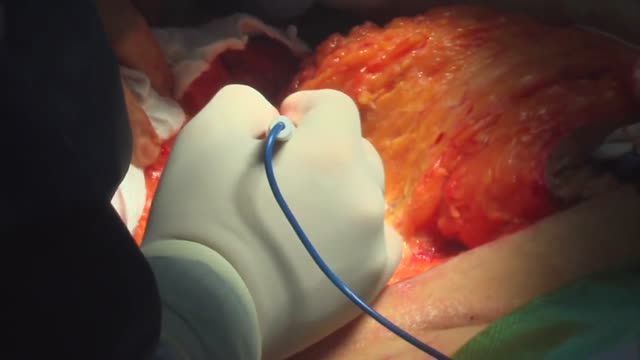
surgical procedure used to remove excess skin and fat from the abdomen and to tighten the muscles of the abdominal wall. Most tummy tuck patients are dealing with the effects of pregnancies and weight loss and find themselves with loose skin in spite of exercise and weight control. Each year, thousands of Americans undergo a tummy tuck to tone, firm and define the abdominal area.

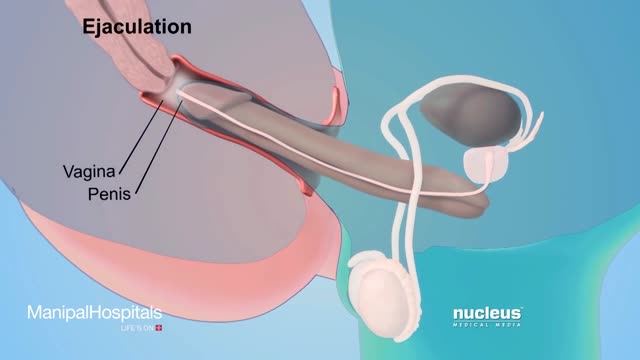
Cases of some sexually transmitted diseases have reached an all-time high, according to a new report from the Centers for Disease Control and Prevention. From 2014 to 2015, there was a 6% increase in diagnosed cases of chlamydia and a 13% increase in gonorrhea.

In this video, the viewer will learn the key aspects of the newborn physical exam, and how to distinguish between normal and abnormal findings.
Direct Links to chapters:
0:00-Intro
1:30-Head
3:49-Face
8:05-Neck
8:30-Chest
10:13-Abdomen
11:01-Groin
13:17-Extremities
14:05-Back
14:47-Neurologic
Please visit: www.openpediatrics.org
OPENPediatrics™ is an interactive digital learning platform for healthcare clinicians sponsored by Boston Children's Hospital and in collaboration with the World Federation of Pediatric Intensive and Critical Care Societies. It is designed to promote the exchange of knowledge between healthcare providers around the world caring for critically ill children in all resource settings. The content includes internationally recognized experts teaching the full range of topics on the care of critically ill children. All content is peer-reviewed and open access-and thus at no expense to the user.
For further information on how to enroll, please email: openpediatrics@childrens.harvard.edu
Please note: OPENPediatrics does not support nor control any related videos in the sidebar, these are placed by Youtube. We apologize for any inconvenience this may cause.

Suspect that a patient has a subphrenic abscess if he deteriorates, or recovers and then deteriorates, between the 14th and the 21st day after a laparotomy, with a low, slowly increasing, swinging fever, sweating, and a tachycardia. This, and a leucocytosis, show that he has ''pus somewhere', which is making him anorexic, wasted, and ultimately cachectic. If he has no sign of a wound infection, a rectal examination is negative, and his abdomen is soft and relaxed, the pus is probably under his diaphragm. The pus might be between his diaphragm and his liver, in (1) his right or (2) his left subphrenic space, or under his liver in (3) his right or (4) his left subhepatic space in his lesser sac. He may have pus in more than one of these spaces. Explore him on the suspicion that he might have a subphrenic abscess. Exploration is not a major operation; the difficulty is knowing where to explore, so refer him if you can. If you cannot refer him, explore him yourself. If you fail to find pus, you have done him no harm; missing a subphrenic abscess is far worse. If it is anterior, you can drain it by going under his costal margin anteriorly. If it is posterior, you can go through the bed of his 12th rib posteriorly.
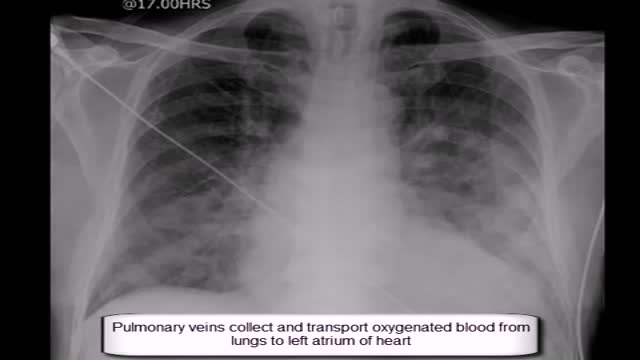
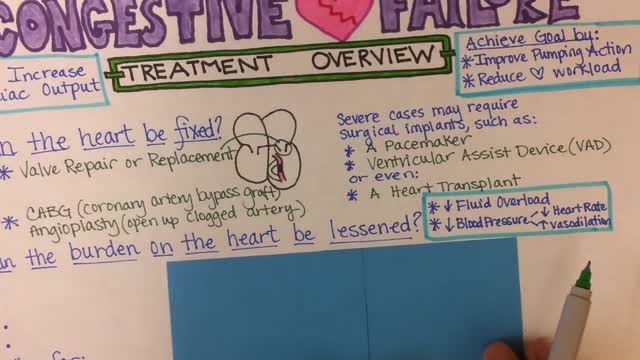
Expand Section. Pulmonary edema is often caused by congestive heart failure. When the heart is not able to pump efficiently, blood can back up into the veins that take blood through the lungs. As the pressure in these blood vessels increases, fluid is pushed into the air spaces (alveoli) in the lungs.

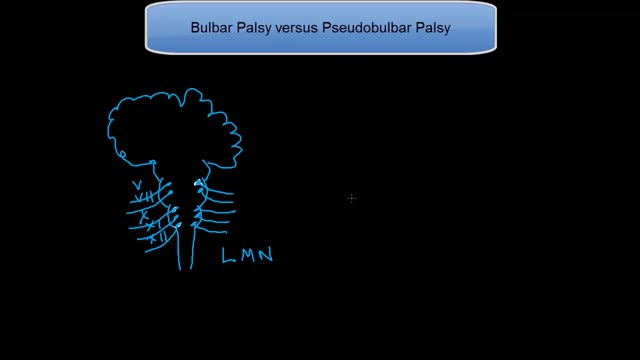
Syringomyelia is a cystic cavitation of the spinal cord associated with Chiari I malformation (70%) or basilar invagination (10%) or tumor. It may be a post-traumatic condition. There are 2 main forms: communicating with the central canal or subarachnoid spaces (Chiari I malformation); non communicating (trauma, tumors).
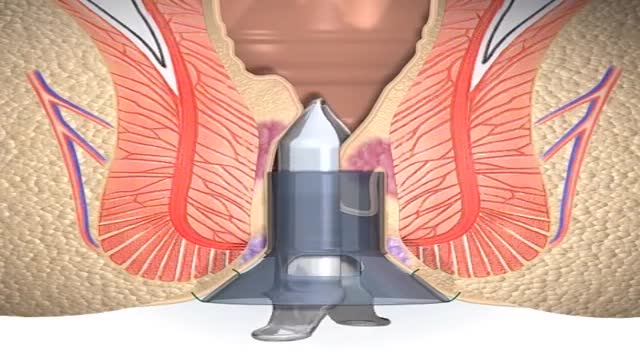
A stapled haemorrhoidopexy is an operation to return the haemorrhoids to a normal. position inside the rectum (back passage). A circular shaped stapling device is gently. inserted in the back passage. The surgeon is then able to use the device to remove.
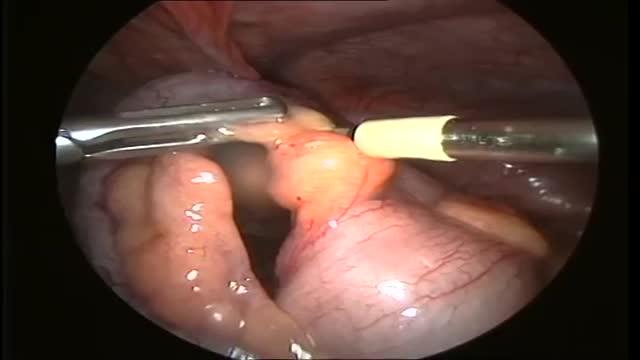
One thing we do know: We can live without it, without apparent consequences. Appendicitis is a medical emergency that requires prompt surgery to remove the appendix. Left untreated, an inflamed appendix will eventually burst, or perforate, spilling infectious materials into the abdominal cavity.

This video shows the technique of suprapatellar tibial nailing as used for a segmental tibia fracture. The broken leg was treated with the nail to allow immediate mobility and range of motion; no cast was needed for this injury.

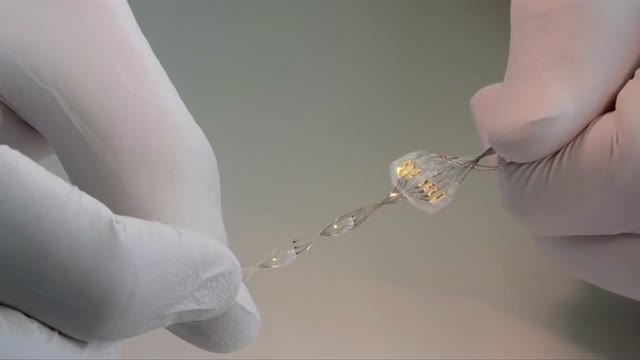
Instead of permanently joining (fusing) vertebrae with metal rods and screws, and therefore restricting movement, the new procedure uses the Anatomic Facet Replacement System (AFRS) device that attaches to each of two adjacent vertebrae with a movable joint that mimics the spine's natural joint.