Orthopedics
This 40 years old man lost his arm in car turn over in 2015. The video is taken 2 years after replantation. You can see another videos in my site: https://drliaghatclinic.com, https://instagram.com/liaghatclinic, https://t.me/liaghatclinic

A 28 years old man lost his right arm with a conveyor device in 2014. The video is taken 2 years after replantation. You can see another videos in my site: https://drliaghatclinic.com, https://instagram.com/liaghatclinic, https://t.me/liaghatclinic

A 29 years old man lost his left wrist in car turn over in 2014. this video is taken 1 year after replantation. You can see another videos in my site: https://drliaghatclinic.com, https://instagram.com/liaghatclinic, https://t.me/liaghatclinic

This 35 years old man lost his right wrist in metal lathe cut machine. the video is taken about 2 years after replantation. You can see another videos in my site: https://drliaghatclinic.com, https://instagram.com/liaghatclinic, https://t.me/liaghatclinic
This 21 years old man lost his right thumb during a street fight sword blow. the video was taken 3 months after replantation. You can see another videos in my site: https://drliaghatclinic.com, https://instagram.com/liaghatclinic, https://t.me/liaghatclinic
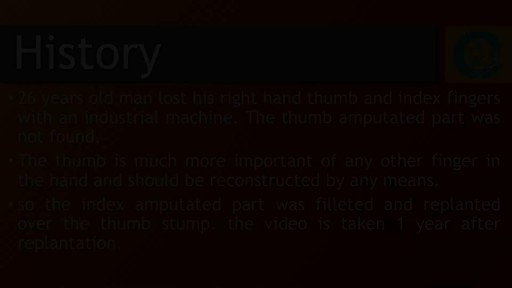
26 years old man lost his right hand thumb and index fingers with an industrial machine.the thumb amputated part was not found. the thumb is much more important of any other finger in the hand and should be reconstructed by any means. so the index amputated part was filleted and replanted over the thumb stump. the video is taken 1 year after replantation. You can see another videos in my site: https://drliaghatclinic.com, https://instagram.com/liaghatclinic, https://t.me/liaghatclinic

This 24 years old man amputated his left hand’s thumb, index, middle and ring fingers with a power saw in 2015. Pre-operative photographies are presented. The video shows the results 7 months after replantation. You can see another videos in my site: https://drliaghatclinic.com, https://instagram.com/liaghatclinic, https://t.me/liaghatclinic

If you look at someone’s back, you’ll see that the spine runs straight down the middle. When a person has scoliosis, their backbone curves to the side. The angle of the curve may be small, large or somewhere in between. But anything that measures more than 10 degrees is considered scoliosis. Doctors may use the letters “C” and “S” to describe the curve of the backbone. You probably don’t look directly at too many spines, but what you might notice about someone with scoliosis is the way they stand. They may lean a little or have shoulders or hips that look uneven. What Causes Scoliosis? In as many as 80% of cases, doctors don’t find the exact reason for a curved spine. Scoliosis without a known cause is what doctors call “idiopathic.” Some kinds of scoliosis do have clear causes. Doctors divide those curves into two types -- structural and nonstructural. In nonstructural scoliosis, the spine works normally, but looks curved. Why does this happen? There are a number of reasons, such as one leg’s being longer than the other, muscle spasms, and inflammations like appendicitis. When these problems are treated, this type of scoliosis often goes away. In structural scoliosis, the curve of the spine is rigid and can’t be reversed
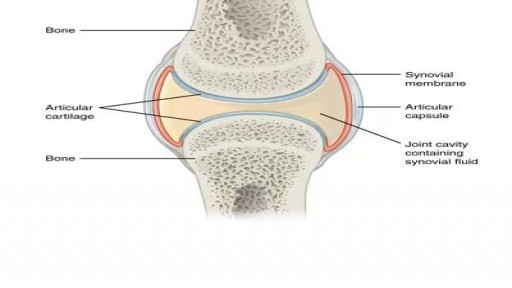
Joint Replacement Surgery is part of Orthopedics hence surgical as well as non-surgical techniques are carried out by orthopedic surgeons. The burden of pain can be reduced with the help of minimally invasive orthopedic therapies prescribed by doctors. https://goo.gl/VhzaUr

In as many as 80% of cases, doctors don’t find the exact reason for a curved spine. Scoliosis without a known cause is what doctors call “idiopathic.” Some kinds of scoliosis do have clear causes. Doctors divide those curves into two types -- structural and nonstructural. In nonstructural scoliosis, the spine works normally, but looks curved. Why does this happen? There are a number of reasons, such as one leg’s being longer than the other, muscle spasms, and inflammations like appendicitis. When these problems are treated, this type of scoliosis often goes away.

Hardware removals are among the most commonly performed surgical procedures worldwide. Current literature offers little data concerning postoperative patient satisfaction. The purpose of our study was to evaluate the patients’ point of view on implant removal. watch to learn more.

- elbow dislocations in children are a relatively uncommon; - peak incidence occurs in adolescence between 11-15 years. - posterior dislocations are most common type; - posterior dislocation usually results from fall on outstretched hand w/ forarm supinated & elbow extended or partially flexed; - coronoid process, which nl resists posterior displacement of ulna, is relatively small in children; - anterior capsule of elbow joint is torn by force of the impact transmitted upward thru the ulna and radius

the elbow is the second most frequently dislocated major joint, after the shoulder. It is the most commonly dislocated joint in children. [1] More than 90% of all elbow dislocations are posterior dislocations. This injury entails disengagement of the coronoid process of the ulna from the trochlea of the humerus with movement posteriorly. [2] The mechanism of injury is typically a fall onto an outstretched hand (FOOSH) with the elbow in extension upon impact.

A boxer's fracture is a break through the bones of the hand that form the knuckles. Some doctors use the term "brawler's fracture" rather than "boxer's fracture" because a boxer is not likely to get this injury. The less well-trained brawlers have to learn how to punch without hurting themselves. The metacarpal bones in the hand connect the bones in the finger to the bones in the wrist. There are five metacarpal bones, one to connect each finger to the wrist. All of the metacarpal bones have the same anatomic structure. Each consists of the base, the shaft, the neck, and the head
Finger metacarpophalangeal (MCP) joint collateral ligament sprains should not be overtreated. First-degree sprains may require a brief period of protection, usually consisting of buddy taping for 2-3 weeks. Second-degree sprains are immobilized in mid flexion for 3 weeks. Finger MCP joint hyperextension injuries may be treated by gently flexing the proximal phalanx and immobilizing the MCP joint in 30° of flexion for 2-3 weeks. A dorsal extension-block splint protects the healing volar plate while allowing active flexion of the finger. Early protected motion minimizes postinjury stiffness. Thumb MCP joint hyperextension injuries ("locked MCP joint") are immobilized in 20° MCP joint flexion for 3 weeks.

Every year, thousands of conventional total shoulder replacements are successfully done in the United States for patients with shoulder arthritis. This type of surgery, however, is not as beneficial for patients with large rotator cuff tears who have developed a complex type of shoulder arthritis called "cuff tear arthropathy." For these patients, conventional total shoulder replacement may result in pain and limited motion, and reverse total shoulder replacement is a better option.

Posterior dislocations with associated fractures, also known as complex posterior dislocations, often require open reduction and fixation (ORIF). These dislocations are often associated with significant ligamentous injury. In some cases, complex posterior elbow dislocations may be managed with closed reduction. Posterior elbow dislocations that are neglected, as is not uncommon in developing countries, can often be effectively treated with open reduction. [9] Delayed vascular compromise is an important complication after reduction. All patients should be observed for a period of approximately 2-3 hours after reduction. If no evidence of vascular compromise arises, patients can be sent home with appropriate follow-up and instructions to watch for further problems.