Orthopedics
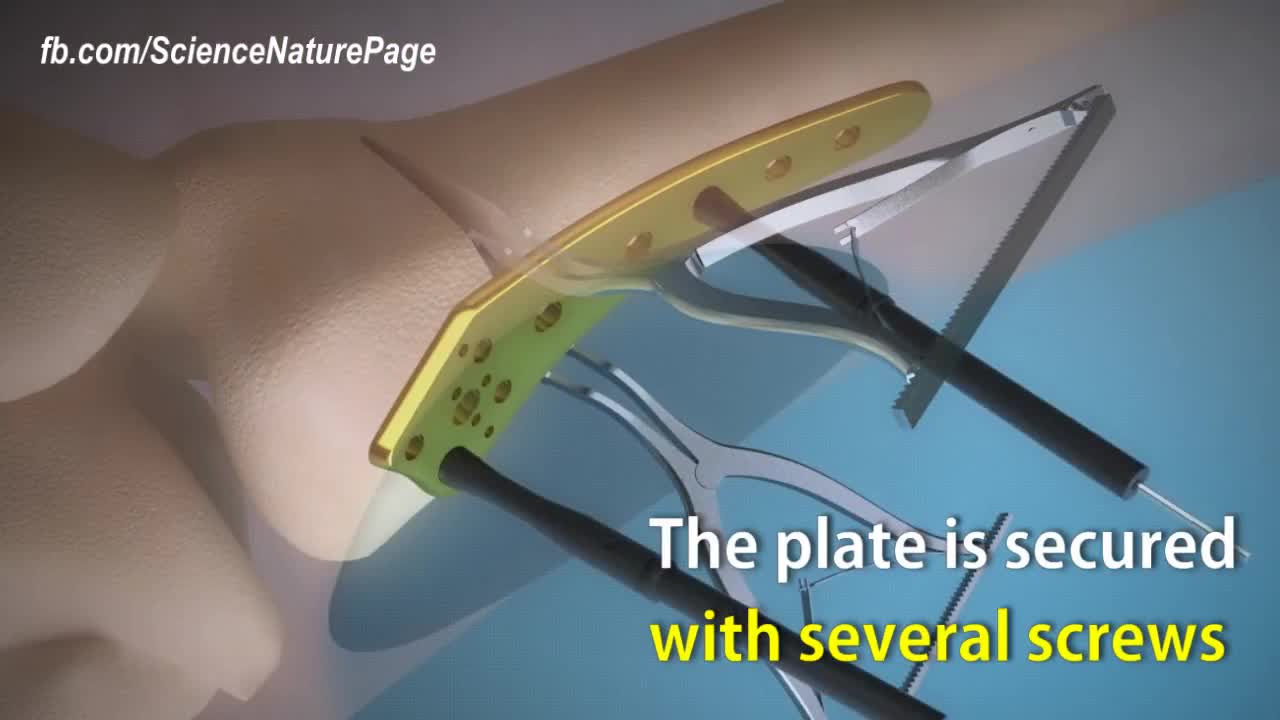
Here is how surgeons perform knock knee correction surgery. Titanium plate is used to stabilize the affected area. The femur is cut nearly through to help with the stability. Spreaders angle the cut align the leg. The plate is secured with several screws. Synthetic bone graft material is packed in the joint. The patient will be in crutches for 4 to 6 weeks.
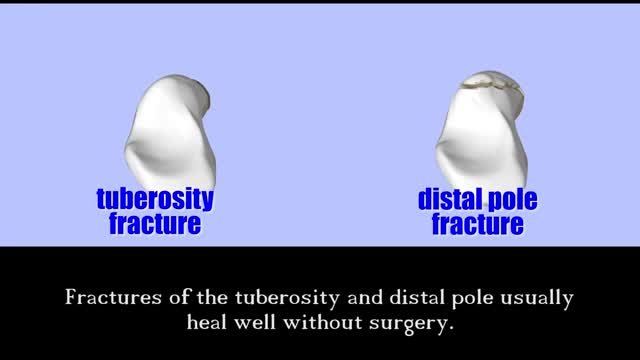
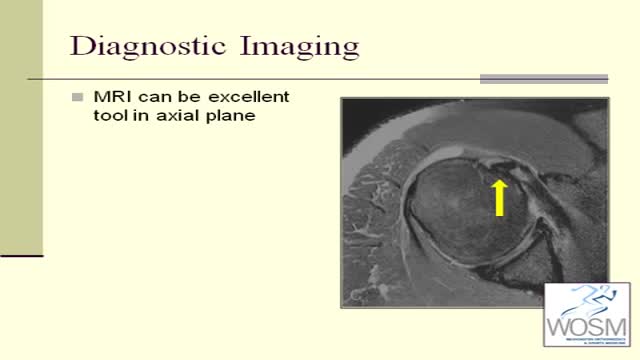
Despite the effective diagnostic and treatment options available today, Dr. Wolfe notes that he continues to see a high number of untreated scaphoid fractures that have progressed to nonunion. However, he adds that this may not be the result of a missed diagnosis, but rather more related to the relatively innocuous injury that causes a low level of suspicion. Recognition and awareness of scaphoid fractures is higher today among primary care providers, emergency room physicians, pediatricians, and sports trainers, but fully 15% of patients with suggestive physical findings and normal initial x-rays will have an “occult”, or concealed, scaphoid fracture. Specialized imaging studies are critical at an early stage to reduce the chance of scaphoid nonunion.

Instead of permanently joining (fusing) vertebrae with metal rods and screws, and therefore restricting movement, the new procedure uses the Anatomic Facet Replacement System (AFRS) device that attaches to each of two adjacent vertebrae with a movable joint that mimics the spine's natural joint.

This video shows the technique of suprapatellar tibial nailing as used for a segmental tibia fracture. The broken leg was treated with the nail to allow immediate mobility and range of motion; no cast was needed for this injury.

A ganglion cyst is a tumor or swelling on top of a joint or the covering of a tendon (tissue that connects muscle to bone). It looks like a sac of liquid (cyst). Inside the cyst is a thick, sticky, clear, colorless, jellylike material. Depending on the size, cysts may feel firm or spongy.

De Quervain's tenosynovitis (dih-kwer-VAINS ten-oh-sine-oh-VIE-tis) is a painful condition affecting the tendons on the thumb side of your wrist. If you have de Quervain's tenosynovitis, it will probably hurt when you turn your wrist, grasp anything or make a fist. Although the exact cause of de Quervain's tenosynovitis isn't known, any activity that relies on repetitive hand or wrist movement — such as working in the garden, playing golf or racket sports, or lifting your baby — can make it worse. Symptoms ShareTweet June 13, 2015 References Products and Services Mayo Clinic Sports Medicine Newsletter: Mayo Clinic Health Letter See also Prednisone risks, benefits Prednisone withdrawal: Why taper down slowly? Integrative approaches to treating pain Lifestyle strategies for pain management Nutrition and pain Pain rehabilitation Self-care approaches to treating pain Show more Advertisement Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Advertising & Sponsorship PolicyOpportunitiesAd Choices Mayo Clinic Store Check out these best-sellers and special offers on books and newsletters from Mayo Clinic. NEW! – The Mayo Clinic Diet, Second Edition Healthy Heart for Life! Mayo Clinic on Better Hearing and Balance Treatment Strategies for Arthritis The Mayo Clinic Diet Online

In a normal hip, the ball at the upper end of the thighbone (femur) fits firmly into the socket, which is part of the large pelvis bone. In babies and children with developmental dysplasia (dislocation) of the hip (DDH), the hip joint has not formed normally.

Possible complications could include: Difficulty healing. Infection. Stump pain (severe pain in the remaining tissue) Phantom limb pain (a painful sensation that the foot or toe is still there) Continued spread of gangrene, requiring amputation of more areas of your foot, toes or leg. Bleeding. Nerve damage.

Pediatric orthopedic surgeons at Columbia are using a new device with magnetic technology that avoids the need for multiple spine-lengthening surgeries to correct early-onset scoliosis, a severe curvature of the spine in young children. In April 2014, Michael Vitale, MD, the Ana Lucia Professor of Pediatric Orthopedic Surgery at CUMC and 1995 graduate of P&S, performed the first procedure in the New York area, using the device to treat a 5-year-old boy. When braces and casts cannot control scoliosis in young children, surgeons turn to growing rods, which help correct the curve while allowing the spine to grow. When spinal maturity is near, the rods are removed and a spinal fusion can be performed. But during years of treatment with growing rods, patients must undergo surgery every six months to lengthen the rods to keep up with the patients’ growth. A patient may undergo eight to 10 procedures, which are costly and result in lost time for parents at work and children at school. The new device—MAGEC (MAGnetic Expansion Control) rods—contains a mechanism inside the growing rods that allows surgeons to lengthen the rods with a handheld external magnet, without surgery.