Orthopedics

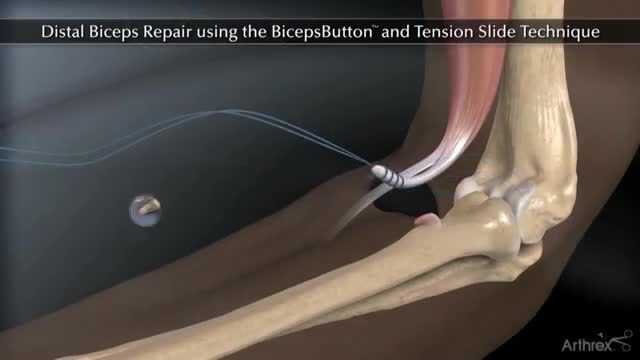
Biceps tenodesis surgery is performed when the biceps tendon is damaged, or the rotator cuff tendon or cartilage ring in the shoulder is torn. The biceps tendon is a strong rope‐like structure connecting the upper end of the biceps muscle to the bones in the shoulder. In biceps tenodesis surgery, the biceps tendon is separated from the shoulder and reattached to the humerus, or the upper arm bone.

The Arthrex® Achilles SpeedBridge™ repair is a surgical technique system that combines fully threaded SwiveLock® anchors with FiberTape® suture. The surgeon may use the Achilles SpeedBridge to reattach the Achilles tendon to the heel bone after repairing the damaged portion of the Achilles tendon. The Achilles tendon connects the two large muscles at the back of the calf to the heel. Insertional Achilles tendinitis is a painful and disabling condition where the tendon attaches to the heel bone causing redness, pain and swelling. Patients who do not respond to the initial treatment may require surgical treatment.
This syndrome was previously known as reflex sympathetic dystrophy, algodystrophy, causalgia, Sudeck atrophy, transient osteoporosis, and acute atrophy of bone. Usually occurring after an injury, CRPS presents with pain out of proportion to the injury, temperature change, edema, and abnormal skin color. Type I CRPS (90% of CRPS cases) occurs without a definable nerve lesion, while type II occurs with a definable nerve lesion. The pathogenesis is likely due to an injury causing increased sensitivity to sympathetic nerves, an abnormal response to and sensation of pain, and increased neuropeptide release causing burning pain to light touch (allodynia).

-Tibial stress fractures are common in athletes and nonathletes who suddenly increase their physical activity. Clinical features include pain, localized tenderness, and swelling. Plain x-ray is <50% sensitive for stress fractures, especially in the first 2-3 weeks after the onset of symptoms. MRI is preferred over bone scan or ultrasound as it can show the fracture line that extends through the cortex into the medullary line. MRI can also identify ligament, muscle, and cartilage injuries. However, MRI findings may be persistently abnormal for up to 1 year after the stress fracture has healed.
A stress fracture typically feels like an aching or burning localized pain somewhere along a bone. Usually, it will hurt to press on it, and the pain will get progressively worse as you run on it, eventually hurting while walking or even when you're not putting any weight on it at all.

McMurray's maneuver is used to detect the presence of meniscal tears. To detect a medial meniscal injury, the patient is put in a supine position with the knee in maximum flexion. One hand of the examiner is placed on the posteromedial margin of the involved knee and the other hand supports the foot. The tibia is then externally rotated, and the knee is extended slowly. The test is positive if there is an audible or palpable click or popping sensation during extension of the involved knee.
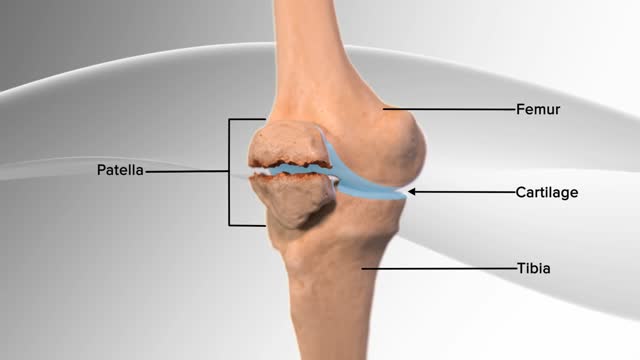
In this knee procedure, the patella is being repaired. The patella is a small, floating bone that glides over the thighbone. It connects the muscles of the thigh to the shinbone, helping the knee to move. The egg‐shell type covering on the underside of the patella and front of the femur allows for smooth motion of the knee.
This new surgical technique provide good stability for all type of fracture even severe comminution. Each fragment are reduced and several pin sleeves are inserted circumferentially and tighten by braded cable through the sleeve box. The final features of surgery seems blooming sunflower 'Himwari in Jananese'.
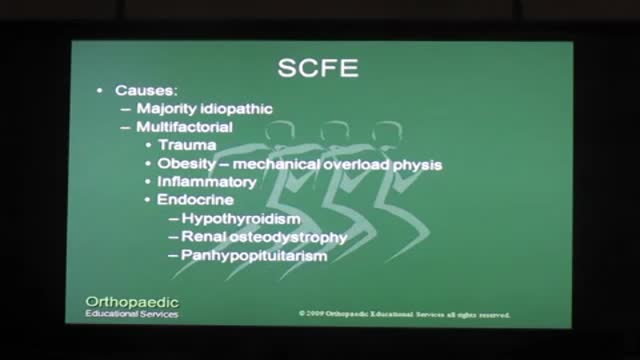
There is a strong association with obesity. In children younger than 10 years, it is associated with metabolic endocrine disorders {hypothyroidism, panhypopituitarism, hypogonadism, renal osteodystrophy, growth hormone abnormalities). SCFE is considered chronic if it has been present more than 3 weeks and acute if it has been present for 3 weeks or less. It is called "stable" if the patient can bear weight and "unstable" if the patient cannot ambulate. Unstable SCFE is associated with more complications, including avascular necrosis of the femoral head (AVN). SCFE is diagnosed by x-ray of the pelvis and bilateral hips. The underlying cause is a widened epiphyseal growth plate, due to abnormal cartilage maturation and endochondral ossification. The treatment is surgical, requiring immediate internal fixation with a single screw. Delay in treatment {> 24 hours) leads to increased AVN, SCFE progression from stable to unstable, and high risk of future degenerative arthritis. Prophylactic contralateral fixation of the unaffected hip is not routinely done in the U.S., except in patients with endocrine abnormalities.
Scoliosis is a sideways curvature of the spine that occurs most often during the growth spurt just before puberty. While scoliosis can be caused by conditions such as cerebral palsy and muscular dystrophy, the cause of most scoliosis is unknown.
If you look at someone’s back, you’ll see that the spine runs straight down the middle. When a person has scoliosis, their backbone curves to the side. The angle of the curve may be small, large or somewhere in between. But anything that measures more than 10 degrees is considered scoliosis. Doctors may use the letters “C” and “S” to describe the curve of the backbone. You probably don’t look directly at too many spines, but what you might notice about someone with scoliosis is the way they stand. They may lean a little or have shoulders or hips that look uneven. What Causes Scoliosis? In as many as 80% of cases, doctors don’t find the exact reason for a curved spine. Scoliosis without a known cause is what doctors call “idiopathic.” Some kinds of scoliosis do have clear causes. Doctors divide those curves into two types -- structural and nonstructural. In nonstructural scoliosis, the spine works normally, but looks curved. Why does this happen? There are a number of reasons, such as one leg’s being longer than the other, muscle spasms, and inflammations like appendicitis. When these problems are treated, this type of scoliosis often goes away.
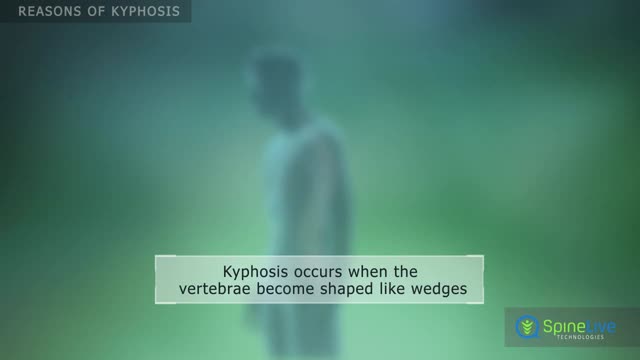
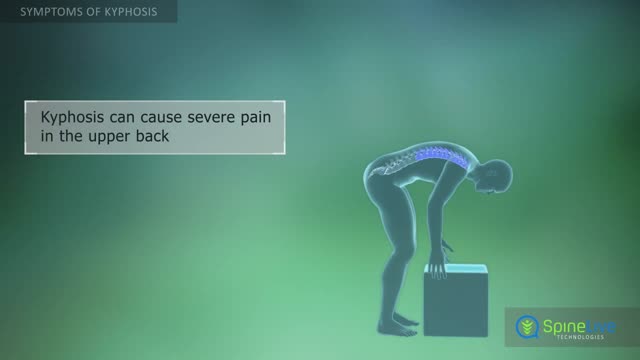
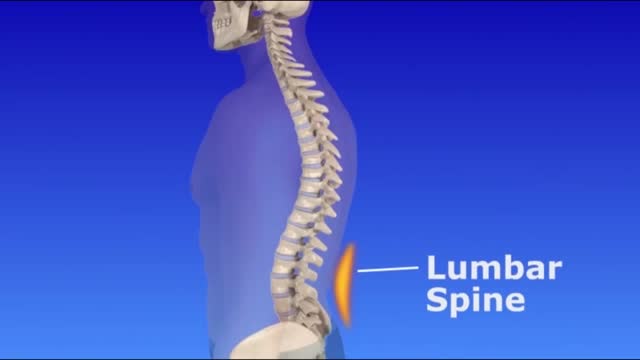
poor posture (postural kyphosis) – slouching, leaning back in chairs and carrying heavy bags can stretch supporting muscles and ligaments, which can increase spinal curvature. abnormally shaped vertebrae (Scheuermann's kyphosis) – if the vertebrae don't develop properly, they can end up being out of position.