Latest videos

The hair transplant surgeon can accurately estimate the number of follicular grafts that can be obtained from dissecting a donor strip of a given size. The same number of follicular units can be used to cover a specific size bald area regardless of the patient's actual hair density.
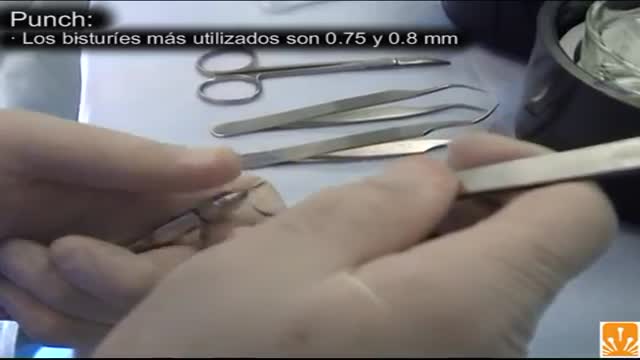
FUE (follicular unit extraction) is a minimally invasive method in hair transplantation. Unlike strip harvesting, the traditional technique in which a strip of skin is removed from a donor site and cut into individual units, FUE uses an instrument to remove multiple groups of one to four hairs. The great thing about FUE is that there’s no linear scar. The downside is that a fewer number of hair grafts can be gathered per session.
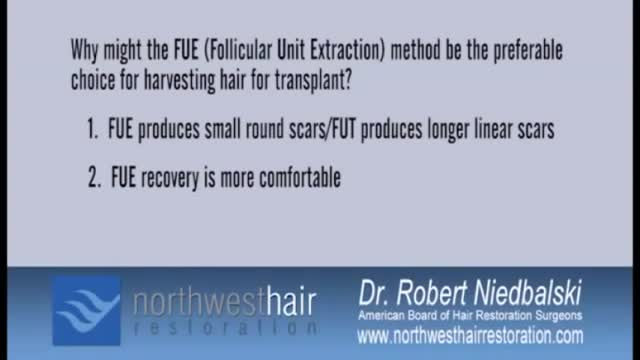
Today, hair transplant physicians are able to make use of different techniques to extract and transplant large numbers of hair follicles (follicular units). There are two primary techniques for hair transplantation currently in use. The FUE (Follicular Unit Extraction) and the FUT (Follicular Unit Transplantation) methods. They differ primarily in the way hair follicles are extracted from the donor area. Follicular Unit Transplantation (FUT) The FUT process involves removing a small strip of tissue from the back of the head, from which the donor hair follicles will be extracted. The hair follicles are harvested from the strip by a skilled clinical team before being individually transplanted to the recipient areas. In most cases, and especially cases of advanced hair loss, FUT is the preferred method because it allows the physician to fully utilize the scalp area to deliver results consistent with patient expectations. FUT typically allows for the greatest number of grafts to be transplanted in a single session. Pain Management Some patients report higher levels of discomfort with FUT procedures compared to FUE due the potential swelling in the area where the strip of tissue was removed, but both methods have a very manageable recovery period and pain medication can be prescribed by your physician if needed. Both techniques of hair transplantation are relatively simple. Hair transplantation procedures are outpatient surgeries with some patients going back to work as soon as the very next day. Scarring The FUT strip extraction method typically results in a very narrow linear scar in the back of the head (typically 1mm in diameter or less in size). Since the scar is very thin, it’s easily concealed by all but the shortest of haircut styles. A short to moderate crop setting on most clippers is sufficient to conceal the scar for the majority of patients, and over time the scar will become less noticeable as it fades. Costs The industry norm for pricing is on a per-graft basis. This allows each individual to pay for only what they need and receive in number of grafts, and not a flat rate that in the end may cost you more. The per-graft cost of a FUT procedure is generally lower than that of a FUE procedure. Lately however, in response to the rising popularity of the FUE technique, many hair transplantation clinics have started lowering the per graft cost on FUE procedures, so that the cost difference between the two types of procedure are not as much as most people think. The costs of medical procedures always vary by patients’ conditions, needs and objectives. For the most accurate assessment of your hair loss and the associated cost of your hair restoration, you will need to speak to a physician. Follicular Unit Extraction (FUE) In an FUE hair transplantation, each follicular unit is individually taken directly from the scalp with no strip of tissue being removed. Hair follicles are removed in a random fashion and the result is less density in the donor area that many say is not even noticeable. This is the main difference between FUE & FUT. Since follicles are removed one at a time, fewer follicles can be harvested during a typical session, making FUE a better option to restore hair in smaller cases (number of grafts) compared to the traditional FUT method. FUE is constantly evolving and what was once utilized for only smaller cases is now being utilized for larger and larger cases. Some people that prefer the FUE method may have the option of splitting their procedure into two days in order to complete their recommended transplantation goals. Pain Management With no stitches required and no linear scar left to heal, FUE procedures do have a faster healing time and less post-procedure discomfort compared to the traditional FUT procedure. Scarring Since FUE procedures involve removing hairs individually from the scalp, there is no linear scar left behind. However, there will be tiny 1mm in diameter or less puncture marks that tend to heal by themselves after scabbing-over in the days following the procedure. These tiny wounds typically heal within three to seven days. Costs Since the physician must remove each hair follicle individually, the time-sensitive nature of an FUE procedure typically makes it more expensive than an FUT procedure. As stated earlier, FUE technology is improving as well as gaining popularity and many hair restoration practices (including Bosley) have started to lower the cost per graft price for FUE procedures. Nowadays, the cost difference between a FUE and a FUT procedures is less disparate.

Surgeons at The Children’s Hospital of Philadelphia were the first to perform a bilateral hand transplant on a child. Our research and work in this groundbreaking field of medicine led us to establish the Hand Transplantation Program. Combining the expertise of the Penn Transplant Institute and the Hospital’s Division of Plastic and Reconstructive Surgery and Division of Orthopedics, the program aims to improve quality of life for children who may benefit from this procedure. This is Zion, one year after the surgery

Surgeons at The Children’s Hospital of Philadelphia were the first to perform a bilateral hand transplant on a child. Our research and work in this groundbreaking field of medicine led us to establish the Hand Transplantation Program. Combining the expertise of the Penn Transplant Institute and the Hospital’s Division of Plastic and Reconstructive Surgery and Division of Orthopedics, the program aims to improve quality of life for children who may benefit from this procedure.

More than three decades on from its first outbreak, HIV/AIDS remains a prevalent killer, even in the developed world, and a pressing scientific challenge to understand and treat. The rate of infection, especially among young people, is increasing, and in parts of Africa in particular, it remains an epidemic-scale killer. Yet a cure could be just around the corner, and scientists are optimistic that the virus’ days might be numbered. Is HIV here to stay, or will it be consigned to history like Smallpox? Produced by ABC Australia - Ref-6621 Journeyman Pictures brings you highlights from the cutting-edge science series, ‘Catalyst’, produced by our long-term content partners at ABC Australia. Every day we’ll upload a new episode that takes you to the heart of the most intriguing and relevant science-related stories of the day, transforming your perspective of the issues shaping our world.
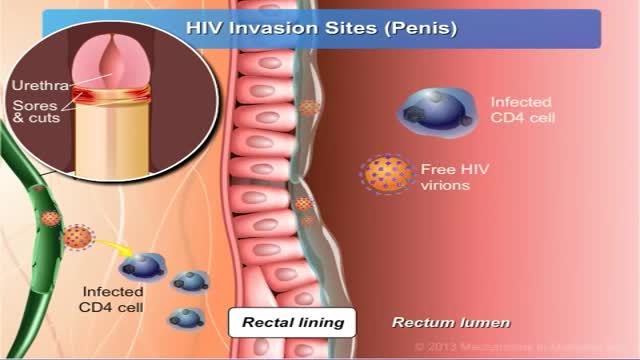
HIV is spread only in certain body fluids from a person infected with HIV. These fluids are blood, semen, pre-seminal fluids, rectal fluids, vaginal fluids, and breast milk. In the United States, HIV is spread mainly by having sex or sharing injection drug equipment, such as needles, with someone who has HIV. To reduce your risk of HIV infection, use condoms correctly every time you have vaginal, oral, or anal sex. Don’t inject drugs. If you do, use only sterile injection equipment and water and never share your equipment with others. Pre-exposure prophylaxis (PrEP) is an HIV prevention option for people who don’t have HIV but who are at high risk of becoming infected with HIV. PrEP involves taking a specific HIV medicine every day. PrEP should always be combined with other prevention options, such as condoms.
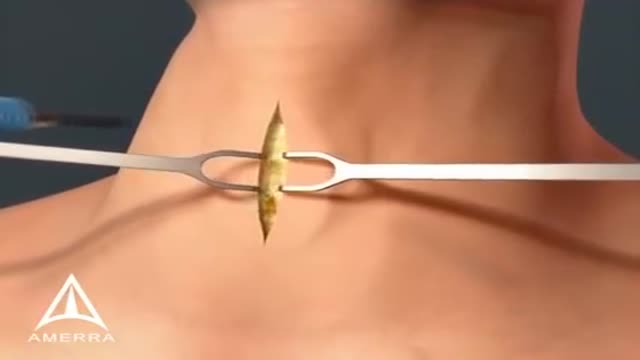
Tracheotomy is a surgical procedure which consists of making an incision on the anterior aspect of the neck and opening a direct airway through an incision in the trachea (windpipe). The resulting stoma (hole), or tracheostomy, can serve independently as an airway or as a site for a tracheostomy tube to be inserted; this tube allows a person to breathe without the use of his or her nose or mouth. Both surgical and percutaneous techniques are widely used in current surgical practice. It is among the oldest described procedures.

A subdural hematoma (SDH) is a collection of blood below the inner layer of the dura but external to the brain and arachnoid membrane (see the images below). Subdural hematoma is the most common type of traumatic intracranial mass lesion. Subdural hematoma occurs not only in patients with severe head injury but also in patients with less severe head injuries, particularly those who are elderly or who are receiving anticoagulants. Subdural hematoma may also be spontaneous or caused by a procedure, such as a lumbar puncture (see Etiology). Rates of mortality and morbidity can be high, even with the best medical and neurosurgical care (see Prognosis). Subdural hematomas are usually characterized on the basis of their size and location and the amount of time elapsed since the inciting event age (ie, whether they are acute, subacute, or chronic). When the inciting event is unknown, the appearance of the hematoma on neuroimaging studies can help determine when the hematoma occurred. These factors, as well as the neurologic and medical condition of the patient, determine the course of treatment and may also influence the outcome. Generally, acute subdural hematomas are less than 72 hours old and are hyperdense compared with the brain on computed tomography scans. The subacute phase begins 3-7 days after acute injury. Chronic subdural hematomas develop over the course of weeks and are hypodense compared with the brain. However, subdural hematomas may be mixed in nature, such as when acute bleeding has occurred into a chronic subdural hematoma. Presentation varies widely in acute subdural hematoma (see Clinical). Many of these patients are comatose on admission. However, approximately 50% of patients with head injuries who require emergency neurosurgery present with head injuries that are classified as moderate or mild (Glasgow Coma Scale scores 9-13 and 14-15, respectively). Many of these patients harbor intracranial mass lesions. In a large series of patients who developed intracranial hematomas requiring emergent decompression, more than half had lucid intervals and were able to make conversation between the time of their injury and subsequent deterioration. In a more comprehensive review of the literature on the surgical treatment of acute subdural hematomas, lucid intervals were noted in up to 38% of cases. These patients may be more likely to benefit from medical and surgical intervention when instituted in a timely fashion (ie, before further neurological deterioration).
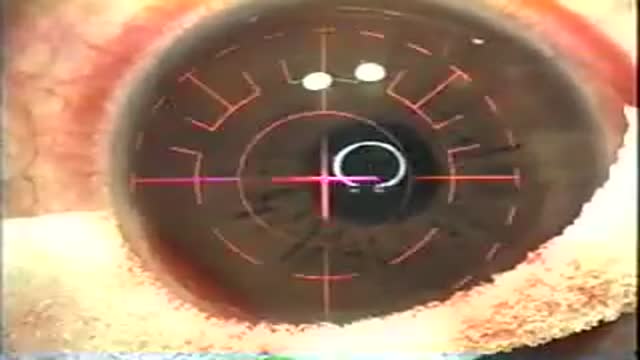
LASIK, which stands for laser in-situ keratomileusis, is a popular surgery used to correct vision in people who are nearsighted, farsighted, or have astigmatism. All laser vision correction surgeries work by reshaping the cornea, the clear front part of the eye, so that light traveling through it is properly focused onto the retina located in the back of the eye. LASIK is one of a number of different surgical techniques used to reshape the cornea.

Ganglion Cyst Volar Wrist Removal Ganglion cysts are noncancerous lumps that most commonly develop along the tendons or joints of your wrists or hands. They also may occur in the ankles and feet. Ganglion cysts are typically round or oval and are filled with a jellylike fluid. Small ganglion cysts can be pea-sized, while larger ones can be around an inch (2.5 centimeters) in diameter. Ganglion cysts can be painful if they press on a nearby nerve. Their location can sometimes interfere with joint movement. If your ganglion cyst is causing you problems, your doctor may suggest trying to drain the cyst with a needle. Removing the cyst surgically also is an option. But if you have no symptoms, no treatment is necessary. In many cases, the cysts go away on their own.

Not every woman undergoes a traditional vaginal delivery with the birth of her child. Under conditions of fetal or maternal distress, or in the case of breech presentation (when a baby is turned feet first at the time of delivery), or if the woman’s first baby was born by cesarean delivery, a procedure called a cesarean section may be required. During a cesarean, a doctor will make either a lateral incision in the skin just above the pubic hair line, or a vertical incision below the navel. As the incision is made, blood vessels are cauterized to slow bleeding. After cutting through the skin, fat, and muscle of the abdomen, the membrane that covers the internal organs is opened, exposing the bladder and uterus. At this time the physician will generally insert his or her hands into the pelvis in order to determine the position of the baby and the placenta. Next, an incision is made into the uterus and any remaining fluids are suctioned from the uterus. The doctor then enlarges the incision with his or her fingers. The baby’s head is then grasped and gently pulled with the rest of its body from the mother’s uterus. Finally, the abdominal layers are sewn together in the reverse order that they were cut. The mother is allowed to recover for approximately three to five days in the hospital. She will also be quite sore and restricted from activity for the following several weeks. There are several potential complications associated with this procedure that should be discussed with a doctor prior to surgery.
The majority of fetuses are in a breech presentation early in pregnancy. By week 38th week of gestation, however, the fetus normally turns to a cephalic presentation. Although the fetal head is the widest single diameter, the fetus’s buttocks [ breech], plus the lower extremities, actually takes up more space. The fundus, being the largest part of the uterus, probably accounts for the fact that in approximately 97% of all pregnancies, the fetus turns so that the buttocks and lower extremities are in the fundus. Vaginal delivery of a breech presentation requires great skill if the fetus is not to be damaged. With the low rate of vaginal breech deliveries in the developed world, experience is being lost. 6% of women with breech presentation still have a vaginal breech delivery as they present too late - so units need to retain a high level of preparedness. Types of breech presentation: I. Complete breech [ flexed breech]: The fetal attitude is one of complete flexion, with hips and knees both flexed and the feet tucked in beside the buttocks. The presenting part consists of two buttocks, external genitalia and two feet. It is commonly present in multiparae. II. Incomplete breech: This is due to varying degrees of extension of thighs or legs at podalic pole. Three varieties are possible; - Breech with extended legs [ frank breech ]: The breech presents with the hips flexed and legs extended on the abdomen. 70% of breech presentations are of this type and it is particularly common in primigravidae whose good uterine muscle tone inhibits flexion of the legs and free turning of the fetus. - Footling breech: This is rare. One or both feet present because neither hips nor knees are fully flexed. The feet are lower than the buttocks, which distinguishes it from the complete breech. - Knee presentation: This is very rare. Thighs are extended but the knees are flexed, bringing the knees down to present at the brim.

This is the incredible moment a new-born baby arrived still inside its amniotic sac, completely intact. The tiny infant can be seen moving and stretching still inside the sac, as medics prepare to snip the new born free. The amniotic sac is a thin but durable membrane filled with fluid which helps keep a baby warm and safe from bumps during pregnancy. When it breaks, this is typically referred to as a woman's 'waters breaking' shortly before she gives birth. But in rare cases, less than 1-in-80,000 births, the baby is delivered with the membranes still intact and this is known as a 'caul birth'. Some babies are born with part of the membrane still attached to them, but to be born completely encased in the intact membrane is incredibly rare. Many people still believe the phenomenon to be a good omen for the child's infancy and it is has even been suggested, but not proven, that caul babies will always have a natural affinity for water. The video was taken in Spain on Saturday and captures the rare moment the baby was born with the membrane covering its entire body, just minutes after its twin was delivered normally.

Shoulder dystocia is a specific case of obstructed labour whereby after the delivery of the head, the anterior shoulder of the infant cannot pass below, or requires significant manipulation to pass below, the pubic symphysis. It is diagnosed when the shoulders fail to deliver shortly after the fetal head. Shoulder dystocia is an obstetric emergency, and fetal demise can occur if the infant is not delivered, due to compression of the umbilical cord within the birth canal. It occurs in approximately 0.3-1% of vaginal births. Contemporary management of shoulder dystocia requires a calm operator and a well-thought-out plan of action. It is imperative that if not already present, help is summoned immediately after shoulder dystocia is recognized. This help may include additional nursing staff, an anesthesiologist, a pediatrician or neonatologist and an additional obstetrician or midwife. Future coordination may demonstrate that rapid response teams are best suited to attend to this emergency.

Your baby's sex is set at conception. At around 7 weeks, your baby's internal sex organs – such as ovaries and testes – begin to form in the abdomen. Male and female sex organs and genitalia look the same at this stage because they're derived from the same structures. At around 9 weeks, boys and girls begin to develop differently. In girls, a tiny bud emerges between the tissue of the legs. This bud will become the clitoris. The membrane that forms a groove below the bud separates to become the labia minora and the vaginal opening. By 22 weeks, the ovaries are completely formed and move from the abdomen to the pelvis. They already contain a lifetime supply of 6 million eggs. In boys, the bud develops into the penis and starts to elongate at around 12 weeks. The outer membrane grows into the scrotal sac that will later house the testicles. By 22 weeks, the testes have formed in the abdomen. They already contain immature sperm. Soon they'll begin their descent to the scrotum, but it's a long journey. They'll reach their destination late in pregnancy, or for some boys, after birth. If you're eager to find out whether you're having a girl or a boy, you'll have to wait until you're at least 17 weeks pregnant. That's when the genitals have developed enough to be seen on an ultrasound.