Latest videos
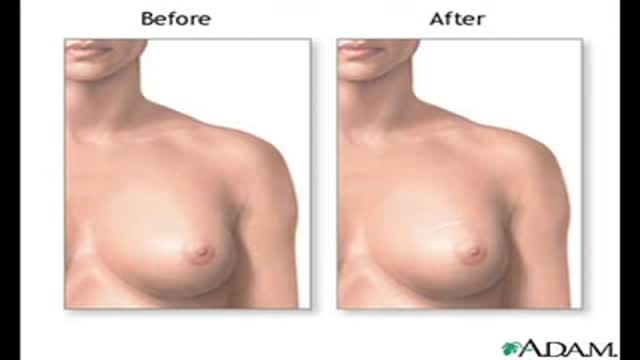
New York Plastic Surgery ,Dr. Robert Vitolo ,board certified plastic surgeon , brings you into the operating room for a glimpse at how his transumbilical breast augmentation procedure is performed. Dr. Vitolo, a pioneer in the 'no visible scar' breast enlargement surgery, has been using this technique since 1994. Dr. Vitolo use Allergan Natrelle saline breast implants and Mentor saline implants. Dr. Vitolo also performs a removal of silicone gel implants and replacement with saline implants using the transumbilical method.
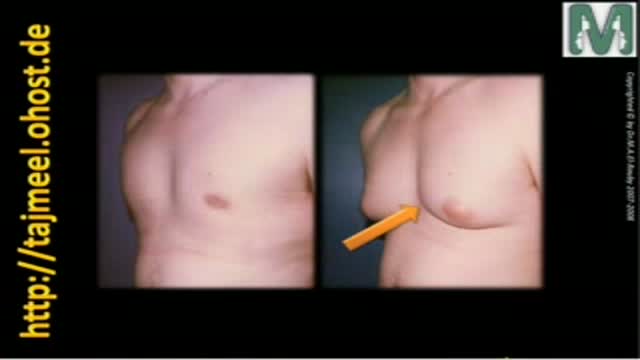
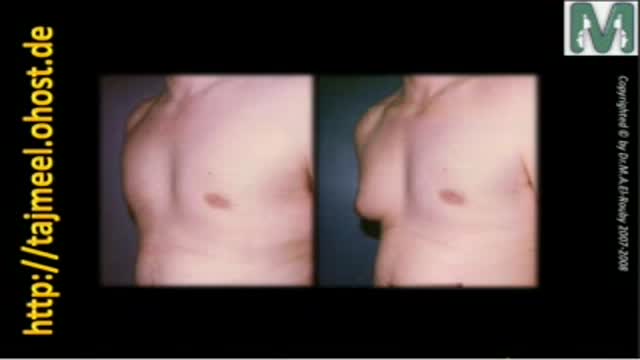
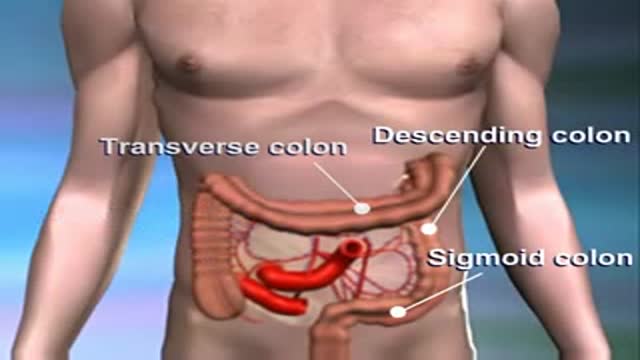
Gynecomastia means enlargement of male breast to resample female breast that is a common problem between males and causes many psychological problem
Dr. Mohamed El-Rouby
Consltant of Plastic surgery - Faculty of Medicine - Ain Shams University