Top videos
Soon enough, a robot will be doing surgeries on you!
Shoulder dystocia is a specific case of obstructed labour whereby after the delivery of the head, the anterior shoulder of the infant cannot pass below, or requires significant manipulation to pass below, the pubic symphysis. It is diagnosed when the shoulders fail to deliver shortly after the fetal head. Shoulder dystocia is an obstetric emergency, and fetal demise can occur if the infant is not delivered, due to compression of the umbilical cord within the birth canal. It occurs in approximately 0.3-1% of vaginal births. Contemporary management of shoulder dystocia requires a calm operator and a well-thought-out plan of action. It is imperative that if not already present, help is summoned immediately after shoulder dystocia is recognized. This help may include additional nursing staff, an anesthesiologist, a pediatrician or neonatologist and an additional obstetrician or midwife. Future coordination may demonstrate that rapid response teams are best suited to attend to this emergency.
The majority of fetuses are in a breech presentation early in pregnancy. By week 38th week of gestation, however, the fetus normally turns to a cephalic presentation. Although the fetal head is the widest single diameter, the fetus’s buttocks [ breech], plus the lower extremities, actually takes up more space. The fundus, being the largest part of the uterus, probably accounts for the fact that in approximately 97% of all pregnancies, the fetus turns so that the buttocks and lower extremities are in the fundus. Vaginal delivery of a breech presentation requires great skill if the fetus is not to be damaged. With the low rate of vaginal breech deliveries in the developed world, experience is being lost. 6% of women with breech presentation still have a vaginal breech delivery as they present too late - so units need to retain a high level of preparedness. Types of breech presentation: I. Complete breech [ flexed breech]: The fetal attitude is one of complete flexion, with hips and knees both flexed and the feet tucked in beside the buttocks. The presenting part consists of two buttocks, external genitalia and two feet. It is commonly present in multiparae. II. Incomplete breech: This is due to varying degrees of extension of thighs or legs at podalic pole. Three varieties are possible; - Breech with extended legs [ frank breech ]: The breech presents with the hips flexed and legs extended on the abdomen. 70% of breech presentations are of this type and it is particularly common in primigravidae whose good uterine muscle tone inhibits flexion of the legs and free turning of the fetus. - Footling breech: This is rare. One or both feet present because neither hips nor knees are fully flexed. The feet are lower than the buttocks, which distinguishes it from the complete breech. - Knee presentation: This is very rare. Thighs are extended but the knees are flexed, bringing the knees down to present at the brim.
No two people alike. Here are the 10 most rare and strange medical conditions all expecting parents dread.
More than three decades on from its first outbreak, HIV/AIDS remains a prevalent killer, even in the developed world, and a pressing scientific challenge to understand and treat. The rate of infection, especially among young people, is increasing, and in parts of Africa in particular, it remains an epidemic-scale killer. Yet a cure could be just around the corner, and scientists are optimistic that the virus’ days might be numbered. Is HIV here to stay, or will it be consigned to history like Smallpox? Produced by ABC Australia - Ref-6621 Journeyman Pictures brings you highlights from the cutting-edge science series, ‘Catalyst’, produced by our long-term content partners at ABC Australia. Every day we’ll upload a new episode that takes you to the heart of the most intriguing and relevant science-related stories of the day, transforming your perspective of the issues shaping our world.
Surgeons at The Children’s Hospital of Philadelphia were the first to perform a bilateral hand transplant on a child. Our research and work in this groundbreaking field of medicine led us to establish the Hand Transplantation Program. Combining the expertise of the Penn Transplant Institute and the Hospital’s Division of Plastic and Reconstructive Surgery and Division of Orthopedics, the program aims to improve quality of life for children who may benefit from this procedure. This is Zion, one year after the surgery
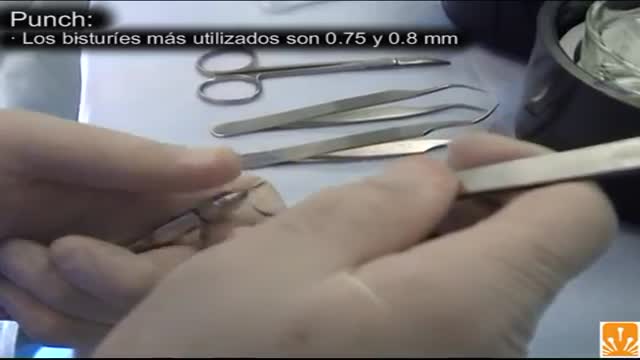
FUE (follicular unit extraction) is a minimally invasive method in hair transplantation. Unlike strip harvesting, the traditional technique in which a strip of skin is removed from a donor site and cut into individual units, FUE uses an instrument to remove multiple groups of one to four hairs. The great thing about FUE is that there’s no linear scar. The downside is that a fewer number of hair grafts can be gathered per session.
The hair transplant surgeon can accurately estimate the number of follicular grafts that can be obtained from dissecting a donor strip of a given size. The same number of follicular units can be used to cover a specific size bald area regardless of the patient's actual hair density.
Toxic shock syndrome is a rare, life-threatening complication of certain types of bacterial infections. Often toxic shock syndrome results from toxins produced by Staphylococcus aureus (staph) bacteria, but the condition may also be caused by toxins produced by group A streptococcus (strep) bacteria. Toxic shock syndrome historically has been associated primarily with the use of superabsorbent tampons. However, since manufacturers pulled certain types of tampons off the market, the incidence of toxic shock syndrome in menstruating women has declined. Toxic shock syndrome can affect men, children and postmenopausal women. Risk factors for toxic shock syndrome include skin wounds and surgery.
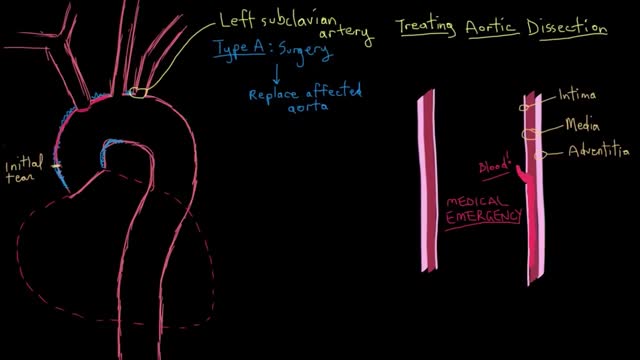
Acute aortic dissection can be treated surgically or medically. In surgical treatment, the area of the aorta with the intimal tear is usually resected and replaced with a Dacron graft. Emergency surgical correction is the preferred treatment for Stanford type A (DeBakey type I and II) ascending aortic dissection. It is also preferred for complicated Stanford type B (DeBakey type III) aortic dissections with clinical or radiologic evidence of the following conditions: Propagation (increasing aortic diameter) Increasing size of hematoma Compromise of major branches of the aorta Impending rupture Persistent pain despite adequate pain management Bleeding into the pleural cavity Development of saccular aneurysm
What is Venipuncture? While venipuncture can refer to a variety of procedures, including the insertion of IV tubes into a vein for the direct application of medicine to the blood stream, in phlebotomy venipuncture refers primarily to using a needle to create a blood evacuation point. As a phlebotomist, you must be prepared to perform venipuncture procedures on adults, children, and even infants while maintaining a supportive demeanor and procedural accuracy. Using a variety of blood extraction tools, you must be prepared to respond to numerous complications in order to minimize the risk to the patient while still drawing a clean sample. In its entirety, venipuncture includes every step in a blood draw procedure—from patient identification to puncturing the vein to labeling the sample. Patient information, needle placement, and emotional environment all play a part in the collection of a blood sample, and it's the fine details that can mean the difference between a definite result and a false positive. After placing the tourniquet and finding the vein, it's time for the phlebotomist to make the complex choice on what procedure will best suit the specific situation. Keeping this in mind, it should be noted that the following information is not an instructional guide on how to perform these phlebotomy procedures. Rather, the information below is intended to serve as an educational resource to inform you of the equipment and procedures you will use. Venipuncture Technqiues Venipuncture with an Evacuated or Vacuum Tube: This is the standard procedure for venipuncture testing. Using a needle and sheath system, this procedure allows multiple sample tubes to be filled through a single puncture. This procedure is ideal for reducing trauma to patients. After drawing the blood, the phlebotomist must make sure the test stopper is correctly coded and doesn't contact exposed blood between samples. Venipuncture with a Butterfly Needle : This is a specialized procedure that utilizes a flexible, butterfly needle adaptor. A butterfly needle has two plastic wings (one on either side of the needle) and is connected to a flexible tube, which is then attached to a reservoir for the blood. Due to the small gauge of the needle and the flexibility of the tube, this procedure is used most often in pediatric care, where the patients tend to have smaller veins and are more likely to move around during the procedure. After being inserted into a vein at a shallow angle, the butterfly needle is held in place by the wings, which allow the phlebotomist to grasp the needle very close to the skin. Phlebotomists should be careful to watch for blood clots in the flexible tubing. Venipuncture with a Syringe: This technique is typically only used when there is a supply shortage, or when a technician thinks it is the appropriate method. It uses the classic needle, tube, and plunger system, operating in a similar manner to the vacuum tube but requiring multiple punctures for multiple samples. Additionally, after the blood is drawn it must be transferred to the appropriate vacuum tube for testing purposes. If you choose to use this method, remember to check for a sterile seal, and use a safety device when transferring the sample. Fingerstick (or Fingerprick): This procedure uses a medical lance to make a small incision in the upper capillaries of a patient's finger in order to collect a tiny blood sample. It is typically used to test glucose and insulin levels. When performing a Fingerstick, the phlebotomist should remember to lance the third or fourth finger on the non-dominant arm. Never lance the tip or the center of the finger pad; instead, lance perpendicular to the fingerprint lines. Heelstick (or Heelprick): Similar to the Fingerstick procedure, this process is used on infants under six months of age. A medical lance is used to create a small incision on the side of an infant's heel in order to collect small amounts of blood for screening. As with a Fingerstick, the incision should be made perpendicular to the heel lines, and it should be made far enough to the left or right side of the heel to avoid patient agitation. Before performing a Heelstick, the infant's heel should be warmed to about 42 degrees Celsius in order to stimulate capillary blood and gas flow. Therapeutic Phlebotomy: This involves the actual letting of blood in order to relieve chemical and pressure imbalances within the blood stream. Making use of a butterfly needle, this therapy provides a slow removal of up to one pint of blood. Though the blood removed is not used for blood transfusions, the procedure and concerns are the same as with routine blood donation. As with any phlebotomy procedure, one should pay close attention to the patient in order to prevent a blood overdraw. Bleeding Time: A simple diagnostic test that is used to determine abnormalities in blood clotting and platelet production. A shallow laceration is made, followed by sterile swabbing of the wound every 30 seconds until the bleeding stops. Average bleed times range between one and nine minutes. As a phlebotomist, you should familiarize yourself with the application and cross-application of these procedures in order to recognize when a procedure is necessary, and what the risks are for each.
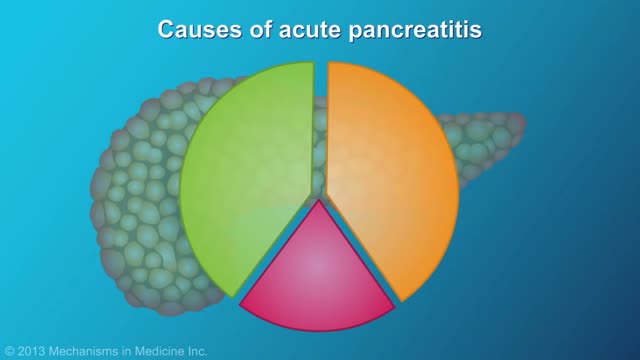
Pancreatitis is inflammation in the pancreas. The pancreas is a long, flat gland that sits tucked behind the stomach in the upper abdomen. The pancreas produces enzymes that assist digestion and hormones that help regulate the way your body processes sugar (glucose). Pancreatitis can occur as acute pancreatitis — meaning it appears suddenly and lasts for days. Or pancreatitis can occur as chronic pancreatitis, which describes pancreatitis that occurs over many years. Mild cases of pancreatitis may go away without treatment, but severe cases can cause life-threatening complications.
Retropharyngeal abscess (RPA) produces the symptoms of sore throat, fever, neck stiffness, and stridor. RPA occurs less commonly today than in the past because of the widespread use of antibiotics for suppurative upper respiratory infections. The incidence of RPA in the United States is rising, however. Once almost exclusively a disease of children, RPA is observed with increasing frequency in adults. It poses a diagnostic challenge for the emergency physician because of its infrequent occurrence and variable presentation.
intracranial hematoma occurs when a blood vessel ruptures within your brain or between your skull and your brain. The collection of blood (hematoma) compresses your brain tissue. An intracranial hematoma may occur because the fluid that surrounds your brain can't absorb the force of a sudden blow or a quick stop. Then your brain may slide forcefully against the inner wall of your skull and become bruised. Although some head injuries — such as one that causes only a brief lapse of consciousness (concussion) — can be minor, an intracranial hematoma is potentially life-threatening and often requires immediate treatment. An intracranial hematoma often, but not always, requires surgery to remove the blood.
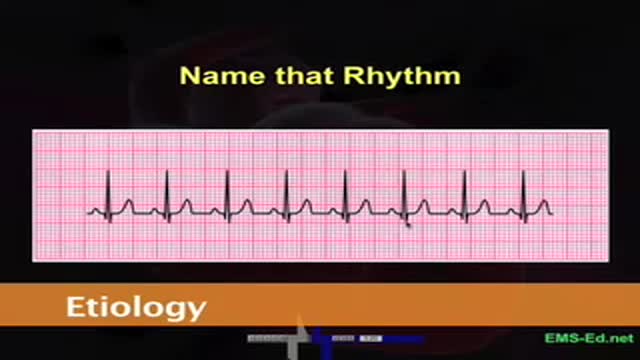
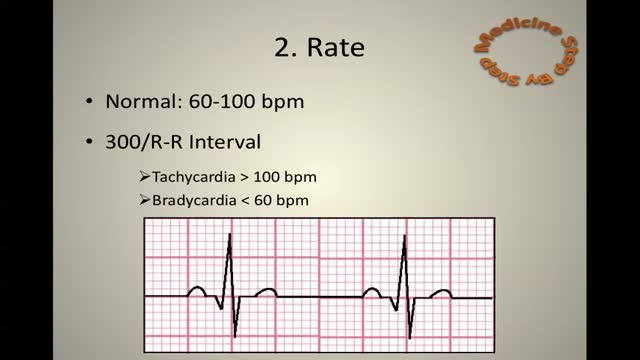
ECG
ECG Learn it
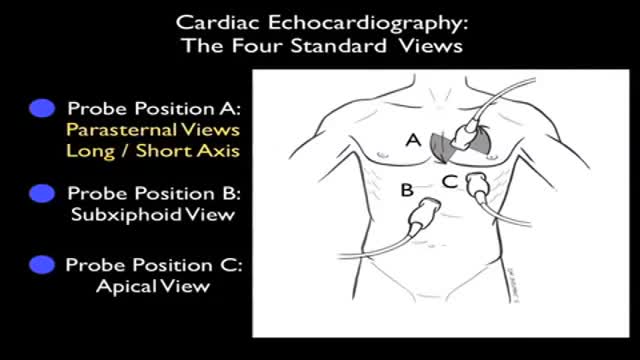
Ultrasound of Heart
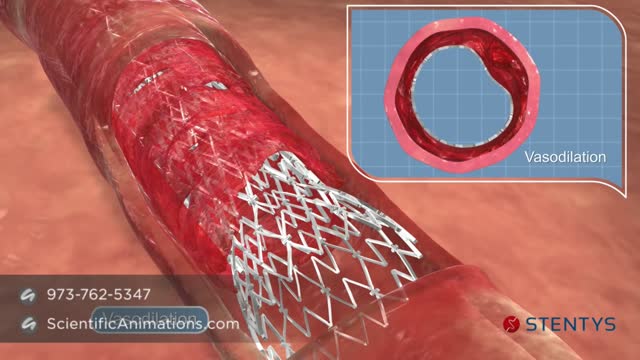
Before the angioplasty procedure begins, you will receive some pain medicine. You may also be given medicine that relaxes you, and blood thinning medicines to prevent a blood clot from forming. You will lie on a padded table. Your doctor will insert a flexible tube (catheter) through a surgical cut into an artery. Sometimes the catheter will be placed in your arm or wrist, or in your upper leg or groin area. You will be awake during the procedure. The doctor will use live x-ray pictures to carefully guide the catheter up into your heart and arteries. Dye will be injected into your body to highlight blood flow through the arteries. This helps the doctor see any blockages in the blood vessels that lead to your heart. A guide wire is moved into and across the blockage. A balloon catheter is pushed over the guide wire and into the blockage. The balloon on the end is blown up (inflated). This opens the blocked vessel and restores proper blood flow to the heart. A wire mesh tube (stent) may then be placed in this blocked area. The stent is inserted along with the balloon catheter. It expands when the balloon is inflated. The stent is left there to help keep the artery open
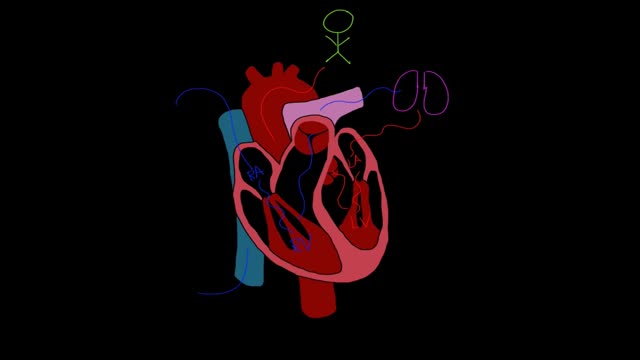
Heart failure, sometimes known as congestive heart failure, occurs when your heart muscle doesn't pump blood as well as it should. Certain conditions, such as narrowed arteries in your heart (coronary artery disease) or high blood pressure, gradually leave your heart too weak or stiff to fill and pump efficiently. Not all conditions that lead to heart failure can be reversed, but treatments can improve the signs and symptoms of heart failure and help you live longer. Lifestyle changes — such as exercising, reducing salt in your diet, managing stress and losing weight — can improve your quality of life. One way to prevent heart failure is to control conditions that cause heart failure, such as coronary artery disease, high blood pressure, diabetes or obesity.
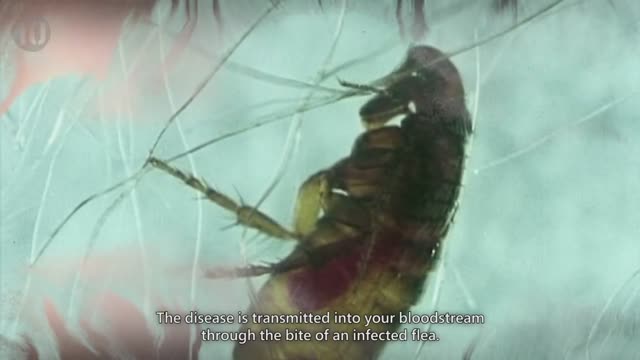
10 Diseases That Will Kill You In A Day