Top videos

It used to be when a woman needed a hysterectomy she could expect full abdominal surgery with a long recovery time. Dr. Melissa Lee uses less invasive methods that can cut the patients downtime in half.
"We were trained in more laparoscopic and minimally invasive cases so of course that's what I'm more comfortable with doing right now."
She sees a new generation of patients opting for laparoscopic surgery.
"Laparoscopy is the use of small cameras with small incisions and instruments that are guided by the hand, and you're able to see directly into the abdomen without actually fully opening the abdomen," says Dr. Lee, an obstetrician-gynecologist with Lee Memorial Health System.
Nowadays, even a large mass or uterus can be removed using the slender tools.
"There are multiple different laparoscopic instruments that you can use. Whether they're blunt dissections or just dissectors that hold and retract back or actual scissors or cutting instruments, there are multiple different options," says Dr. Lee.
While a standard abdominal hysterectomy requires a four to eight inch incision, the laparoscope needs only a quarter to half inch. It's enough to make a big difference in terms of recovery.
"They're able to get up and move around faster. They're able to recover faster, their pain level and their need for pain medicine is much lower," says Dr. Lee.
The laparoscopic procedure also cuts down on scarring and more importantly, shortens the hospital stay. The trend now is home within 24 hours.
"Where the patient is done early in the morning, they're doing well they're tolerating oral intake they're able to getup and move around. And those patients a lot of times will feel comfortable to go home that same nigh after a major surgery," says Dr. Lee.
New studies show women who've had a laparoscopic hysterectomy viewed their quality of life as better than those who had an open abdominal procedure, making this a good option for the right patient.
View More Health Matters video segments at leememorial.org/healthmatters/
Lee Memorial Health System in Fort Myers, FL is the largest network of medical care facilities in Southwest Florida and is highly respected for its expertise, innovation and quality of care. For nearly a century, we've been providing our community with everything from primary care treatment to highly specialized care services and robotic assisted surgeries.
Visit leememorial.org

.
Chapters
0:00 Introduction
1:04 Why do doctors perform laparoscopy?
2:11 How is laparoscopy performed?
3:22 Result
3:47 Risk of laparoscopy
Laparoscopy (from Ancient Greek λαπάρα (lapára) 'flank, side', and σκοπέω (skopéō) 'to see') is an operation performed in the abdomen or pelvis using small incisions (usually 0.5–1.5 cm) with the aid of a camera. The laparoscope aids diagnosis or therapeutic interventions with a few small cuts in the abdomen.[1]
Laparoscopic surgery, also called minimally invasive procedure, bandaid surgery, or keyhole surgery, is a modern surgical technique. There are a number of advantages to the patient with laparoscopic surgery versus an exploratory laparotomy. These include reduced pain due to smaller incisions, reduced hemorrhaging, and shorter recovery time. The key element is the use of a laparoscope, a long fiber optic cable system that allows viewing of the affected area by snaking the cable from a more distant, but more easily accessible location.
Laparoscopic surgery includes operations within the abdominal or pelvic cavities, whereas keyhole surgery performed on the thoracic or chest cavity is called thoracoscopic surgery. Specific surgical instruments used in laparoscopic surgery include obstetrical forceps, scissors, probes, dissectors, hooks, and retractors. Laparoscopic and thoracoscopic surgery belong to the broader field of endoscopy. The first laparoscopic procedure was performed by German surgeon Georg Kelling in 1901. There are two types of laparoscope:[2]
A telescopic rod lens system, usually connected to a video camera (single-chip or three-chip)
A digital laparoscope where a miniature digital video camera is placed at the end of the laparoscope, eliminating the rod lens system
The mechanism mentioned in the second type is mainly used to improve the image quality of flexible endoscopes, replacing conventional fiberscopes. Nevertheless, laparoscopes are rigid endoscopes. Rigidity is required in clinical practice. The rod-lens-based laparoscopes dominate overwhelmingly in practice, due to their fine optical resolution (50 µm typically, dependent on the aperture size used in the objective lens), and the image quality can be better than that of the digital camera if necessary. The second type of laparoscope is very rare in the laparoscope market and in hospitals.[citation needed]
Also attached is a fiber optic cable system connected to a "cold" light source (halogen or xenon) to illuminate the operative field, which is inserted through a 5 mm or 10 mm cannula or trocar. The abdomen is usually insufflated with carbon dioxide gas. This elevates the abdominal wall above the internal organs to create a working and viewing space. CO2 is used because it is common to the human body and can be absorbed by tissue and removed by the respiratory system. It is also non-flammable, which is important because electrosurgical devices are commonly used in laparoscopic procedures.[3]
Procedures
Surgeons perform laparoscopic stomach surgery.
Patient position
During the laparoscopic procedure, the position of the patient is either in Trendelenburg position or in reverse Trendelenburg. These positions have an effect on cardiopulmonary function. In Trendelenburg's position, there is an increased preload due to an increase in the venous return from lower extremities. This position results in cephalic shifting of the viscera, which accentuates the pressure on the diaphragm. In the case of reverse Trendelenburg position, pulmonary function tends to improve as there is a caudal shifting of viscera, which improves tidal volume by a decrease in the pressure on the diaphragm. This position also decreases the preload on the heart and causes a decrease in the venous return leading to hypotension. The pooling of blood in the lower extremities increases the stasis and predisposes the patient to develop deep vein thrombosis (DVT).[4]
Gallbladder
Rather than a minimum 20 cm incision as in traditional (open) cholecystectomy, four incisions of 0.5–1.0 cm, or more recently, a single incision of 1.5–2.0 cm,[5] will be sufficient to perform a laparoscopic removal of a gallbladder. Since the gallbladder is similar to a small balloon that stores and releases bile, it can usually be removed from the abdomen by suctioning out the bile and then removing the deflated gallbladder through the 1 cm incision at the patient's navel. The length of postoperative stay in the hospital is minimal, and same-day discharges are possible in cases of early morning procedures.[citation needed]
Colon and kidney

Dr. Celia Divino, Chief, Division of General Surgery at The Mount Sinai Hospital, performs a laparoscopic appendectomy. Visit the Division of General Surgery at http://bit.ly/18z944M. Click here to learn more about Dr. Celia Divino http://bit.ly/12RF0ee

http://www.laparoscopyhospital.com
For the surgeon to develop the same level of proficiency and dexterity in the endoscopic environment as he may possess in open surgery is not a simple matter. The use of proper Mishra's Knot, are essential. Participating in an in-depth, systematic training program in a laboratory setting is essential before applying endoscopic Mishra's Knot techniques to humans. Successful acquisition of these Mishra's Knot skill requires that the surgeon be motivated to succeed and willing to invest the time and effort necessary to do so. Succumbing to the temptation of mechanical devices in lieu of acquiring the manual skills results in a questionable dependence on disposable technology and reduces the cost effectiveness of the minimally invasive approach. It is the adoption of Mishra's Knotting skills by the surgeon that will expand the surgeon's capability of performing increasingly advanced endoscopic surgical procedures.
For more information please contact:
World Laparoscopy Hospital
Cyber City, DLF Phase II, Gurgaon
NCR Delhi, 122002, India
Phone & WhatsApp: +919811416838, + 91 9999677788
contact@laparoscopyhospital.com
For more information about living liver donor program, please visit https://cle.clinic/31rgy9F
Unlike open surgery that requires a large incision to access the liver, the laparoscopic procedure is performed with surgical tools and a camera inserted through a few half-inch holes in the abdomen of the living donor. Once the piece of the liver is dissected, the surgeon retrieves the graft through a small incision below the navel.
Liver transplant surgeon C.H David Kwon, MD, discusses the laparoscopic liver donor procedure more.
To learn more about Dr. Kwon, please visit https://cle.clinic/3Lvk9cv
If you liked the video hit like and subscribe for more!
#clevelandclinic #livingdonor #livertransplantation #livertransplant #organdonation #laparoscopicsurgeon #laparoscopysurgery

"Laparoscopic Placement of a
Peritoneal Dialysis Catheter"
Houston Methodist DeBakey Heart & Vascular Center, presents a cardiovascular procedure featuring Eric K. Peden, MD, Shri Timbalia, MD, and Kenneth Livingston as they demonstrate “Laparoscopic Placement of a
Peritoneal Dialysis Catheter".
Surgery: Eric K. Peden, MD, Shri Timbalia, MD, and Kenneth Livingston
Narration: Kenneth Livingston
** This medical education program may contain graphic content. **
_________________________________
A DeBakey CV Education event
Presented by Houston Methodist DeBakey Heart & Vascular Center.
Building on Dr. Michael E. DeBakey’s commitment to excellence in education, Houston Methodist DeBakey CV Education is an epicenter for cardiovascular academic and clinical educational programs that support the provision of optimal care to patients suffering from cardiovascular conditions and diseases.
FOR MORE INFORMATION
DeBakey CV Education:
https://www.houstonmethodist.o....rg/education/medical
For the latest education and training opportunities from DeBakey CV Education: http://bit.ly/HMdebakeyemail
Follow Us:
Facebook: https://www.facebook.com/debakeycvedu
Twitter: https://twitter.com/DeBakeyCVedu
Livestream: https://livestream.com/debakey
SmugMug: https://debakey.smugmug.com/
Want concise, relevant reviews of the hottest topics in CV medicine? Subscribe for FREE to the Methodist DeBakey Cardiovascular Journal for quarterly, peer-reviewed issues delivered to your door.
https://journal.houstonmethodist.org/

This video demonstrate Laparoscopic Cholecystectomy Full Length Skin to Skin Video with Infrared Cholangiography performed by Dr R K Mishra at World Laparoscopy Hospital. Infrared Cholegiography is performed by using Indocyanine Green during laparoscopic cholecystectomy surgery for gallbladder removal. Bile duct injury remains the most feared complication of laparoscopic cholecystectomy. Intraoperative cholangiography (IOC) is the current gold standard for biliary imaging and may reduce injury, but is not widely used because of the difficulties of doing it. Near-Infrared Fluorescence Cholangiography (NIRF-C) is a novel non-invasive method for real-time, radiation-free, intra-operative biliary mapping during laparoscopic cholecystectomy. We have experienced that NIRF-C is a safe and effective method for identifying biliary anatomy during laparoscopic cholecystectomy. Indocyanine green is a cyanine dye is very popular and used for many years in medical diagnostics. It is used for determining cardiac output, hepatic function, liver, and gastric blood flow, and for ophthalmic angiography. Now the use of this dye in lap chole has improved the safety of this surgery by NEAR INFRARED FLUORESCENT CHOLANGIOGRAPHY.
For more information please contact:
World Laparoscopy Hospital
Cyber City, Gurugram, NCR DELHI
INDIA 122002
Phone & WhatsApp: +919811416838, + 91 9999677788

http://drraewynteirney.com.au/video/
http://drraewynteirney.com.au/....about-dr-raewyn-teir
Dr Raewyn Teirney - fertility specialist and Gynaecologist in Sydney shows a video recording of a laparoscopy for a woman with infertility and pelvic pain.

Unique 3D technology from Olympus:
http://www.olympus-europa.com/....medical/en/medical_s
Discover the 3rd dimension of endoscopy and experience laparoscopy in a totally new dimension.
Contact us for more information:http://www.olympus-europa.com/....medical/en/medical_s

Dr. Erica Hodgman discusses pediatric surgery at the Johns Hopkins Children's Center Pediatric General Surgery program, what common surgeries the program specializes in, what makes the program unique and her work as a pediatric surgeon. #PediatricSurgery #JohnsHopkinsChildrenCenter
Questions Answered:
0:03 Describe the pediatric general surgery division at Johns Hopkins Children's Center.
1:00 What makes this program unique?
1:31 What are some common pediatric surgery cases?
2:23 Explain your work as a pediatric general surgeon?

Our surgeons take a compassionate, family-centered approach to both inpatient and outpatient care. We’re committed to making sure both you and your child understand our process. Told through a kid's eyes, this video tour reveals our caring approach.
To learn more about pediatric surgery at Stamford Hospital, visit: https://www.stamfordhealth.org..../care-treatment/pedi

Not sure what to expect with your child's upcoming surgery at Wesley Children's Hospital? This guided tour will walk you through the process to make both patients and families feel as comfortable as possible.
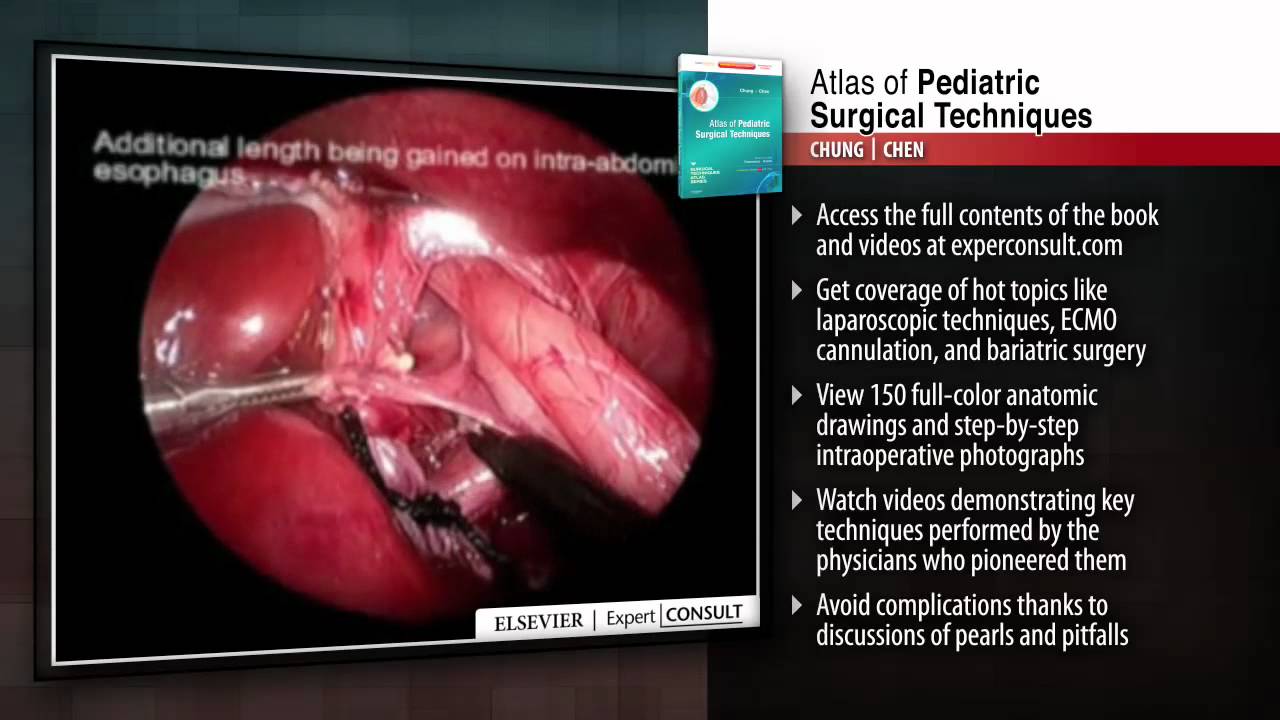
This title in the new Surgical Techniques Atlas series presents state-of-the-art updates on the full range of pediatric surgical techniques performed today. Expand your repertoire and hone your clinical skills thanks to the expert advice, procedural videos, and online access at expertconsult.com. For more information, please visit http://www.us.elsevierhealth.com/product.jsp?sid=EHS_US_BS-SPE-59&isbn=9781416046899&dmnum=null&elsca1=CriticalCare&elsca2=soc_med&elsca3=null&elsca4=youtube_ELSpromovideos
Sanjeev Dutta, MD, FACS discusses the fascinating new world of surgical technology. The pediatric general surgeon shares how medicine and technology have combined to achieve less invasive procedures and healthier outcomes for surgical patients.
Dr. Dutta is a pediatric general surgeon at Lucile Packard Children's Hospital. He is also an Associate Professor of Surgery at Stanford School of Medicine and Surgical Director of the Multidisciplinary Initiative for Surgical Technology Research.
Learn more about Stanford Children's Health. http://www.stanfordchildrens.org.

"I’m essentially taking care of the baby right now to give them 60 or 70 or 80 years of life so I have to perform my best every time. Every single time. That is a commitment that I have to the parents."
The highest standard. That’s what cardiothoracic surgeon Sergio Carrillo demands of himself every time he steps into the OR. Dr. Carrillo and his Heart Center team at Nationwide Children’s Hospital treat patients with congenital heart disease with the simplest to the most complex procedures.
Connect with a specialist: http://bit.ly/2LU2kJn
The Heart Center at Nationwide Children's: http://bit.ly/2LTQmPR
Advancing cardiac care through research: http://bit.ly/2LXFqAD
Tissue Engineering Research & Innovation: http://bit.ly/2LUD0Ts
Heart & Chest Surgery, What to Expect: http://bit.ly/2LVQr5J
Meet our Heart Center Team: http://bit.ly/2LUvdF9

Today, the most common approach for open-heart surgery is a sternotomy, which requires a 12-14-inch incision through the breastbone. But in the hands of experienced minimally invasive surgeons, many cardiac procedures can be performed through smaller 2- to 3-inch incisions between the ribs without the need to cut through the breastbone. Learn more in this medical animation from Sarasota Memorial's Minimally Invasive Cardiac Surgery Team and medical director Jonathan Hoffberger, DO. For information or referrals, visit smhheart.com.

Emory has one of the few heart and vascular centers nationally performing robotic cardiac surgery using the daVinci Surgical System. Emory's robotic surgeons have completed numerous cases and are recognized in Atlanta, the Southeast and across the country for their expertise in cardiac surgery. Some of the cardiac and thoracic conditions treated by Emory cardiac surgeons include mitral valve repair and replacement, atrial septal defect repair, atrial myxoma and thrombi, coronary bypass (LIMA to LAD), mediastinal mass excision, thymectomy, epicardial lead placement and pericardial window.




