Top videos

Physical assessment is taking an educated, systematic look at all aspects of an individual’s health status utilizing knowledge, skills and tools of health history and physical exam. To collect data- information about the client’s health, including physiological, psychological, sociocultural and spiritual aspects To establish actual and potential problems To establish the nurse-client relationship Method: The history is done first, then the physical examination focuses on finding data associated with the history. Health History- obtained through interview and record review. Physical exam- accomplished by tools and techniques ** A complete assessment is not necessarily carried out each time. A comprehensive assessment is part of a health screening examination. On admission, you will do an admission assessment (not necessarily including everything presented here) and document it on the admission form. You will do a daily shift assessment (patient systems review). And, if client has a specific problem, you may assess only that part of the body (focused). Data Collection: Information is organized into objective and subjective data: Subjective: Apparent only to person affected; includes client’s perceptions, feelings, thoughts, and expectations. It cannot be directly observed and can be discovered only asking questions. Objective: Detectable by an observer or can be tested against an acceptable standard; tangible, observable facts; includes observation of client behavior, medical records, lab and diagnostic tests, data collected by physical exam. ** To obtain data for the nursing health history, you must utilize good interview techniques and communications skills. Record accurately. DO NOT ASSUME. D. Frameworks for Health Assessment There are two main frameworks utilized in health assessment: Head to Toe- systematic collection of data starting with the head and working downward. Functional Health Assessment- Gordon’s 11 functional health patterns that address the behaviors a person uses to maintain health. PERSON is the ACC-ADN framework for assessment. It is similar to Gordon's functional health patterns.
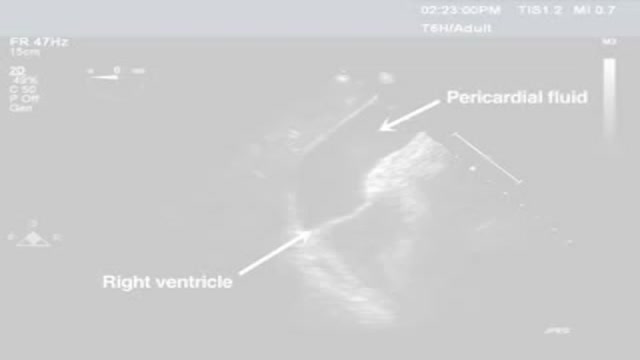
Pericardiocentesis is the aspiration of fluid from the pericardial space that surrounds the heart. This procedure can be life saving in patients with cardiac tamponade, even when it complicates acute type A aortic dissection and when cardiothoracic surgery is not available. [1] Cardiac tamponade is a time sensitive, life-threatening condition that requires prompt diagnosis and management. Historically, the diagnosis of cardiac tamponade has been based on clinical findings. Claude Beck, a cardiovascular surgeon, described 2 triads of clinical findings that he found associated with acute and chronic cardiac tamponade. The first of these triads consisted of hypotension, an increased venous pressure, and a quiet heart. It has come to be recognized as Beck's triad, a collection of findings most commonly produced by acute intrapericardial hemorrhage. Subsequent studies have shown that these classic findings are observed in only a minority of patients with cardiac tamponade. [2] The detection of pericardial fluid has been facilitated by the development and continued improvement of echocardiography. [3] Cardiac ultrasound is now accepted as the criterion standard imaging modality for the assessment of pericardial effusions and the dynamic findings consistent with cardiac tamponade. With echocardiography, the location of the effusion can be identified, the size can be estimated (small, medium, or large), and the hemodynamic effects can be examined by assessing for abnormal septal motion, right atrial or right ventricular inversion, and decreased respiratory variation of the diameter of the inferior vena cava.
With bone marrow disease, there are problems with the stem cells or how they develop: In leukemia, a cancer of the blood, the bone marrow makes abnormal white blood cells. In aplastic anemia, the bone marrow doesn't make red blood cells. In myeloproliferative disorders, the bone marrow makes too many white blood cells.Nov 22, 2016

A visual prosthesis, often referred to as a bionic eye, is an experimental visual device intended to restore functional vision in those suffering from partial or total blindness. In 1983 Joao Lobo Antunes, a Portuguese doctor, implanted a bionic eye in a person born blind.
Surgery to replace an aortic valve is done for aortic valve stenosis and aortic valve regurgitation. During this surgery, the damaged valve is removed and replaced with an artificial valve. The valve replacement is typically an open-heart surgery.
poor posture (postural kyphosis) – slouching, leaning back in chairs and carrying heavy bags can stretch supporting muscles and ligaments, which can increase spinal curvature. abnormally shaped vertebrae (Scheuermann's kyphosis) – if the vertebrae don't develop properly, they can end up being out of position.
Indwelling urinary catheters are commonly used in hospitals and can lead to preventable catheter-associated UTI. How can rates of catheter-associated UTI be reduced in hospitals? New research findings are summarized in a new NEJM Quick Take. Learn more at http://nej.md/1WoeHdF SHOW MORE
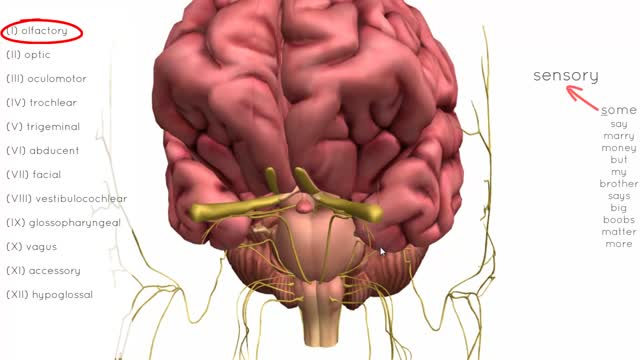
There are twelve cranial nerves in total. The olfactory nerve (CN I) and optic nerve (CN II) originate from the cerebrum. Cranial nerves III – XII arise from the brain stem (Figure 1). They can arise from a specific part of the brain stem (midbrain, pons or medulla), or from a junction between two parts: Midbrain – the trochlear nerve (IV) comes from the posterior side of the midbrain. It has the longest intracranial length of all the cranial nerves. Midbrain-pontine junction – oculomotor (III). Pons – trigeminal (V). Pontine-medulla junction – abducens, facial, vestibulocochlear (VI-VIII). Medulla Oblongata – posterior to the olive: glossopharyngeal, vagus, accessory (IX-XI). Anterior to the olive: hypoglossal (XII). The cranial nerves are numbered by their loca

A VCUG (Voiding Cystourethrogram) is a test that looks at how well your child's kidneys, ureters and bladder are working. Your child's kidneys make urine. The urine flows from the kidneys through thin tubes (called ureters) into your child's bladder.

Delayed puberty is defined as the absence of any signs suggestive of puberty by 14 years of age. In this case, the patient's pubertal delay appears to be constitutional because of his positive family history, absence of syndromic features or systemic illness, and bone age of 12 years. Puberty correlates more closely with bone age than chronological age. On follow-up, the patient will most likely demonstrate a similar onset of puberty as his father.