Top videos

Devi Shetty, founder of Narayana Health in India, reflects on the remarkable fact that, after 26 years of operation, the cost of heart surgery at Narayana Health has come down dramatically, and shares some of the strategies used to maintain high quality with low patient cost.
Learn more about the Creating Emerging Markets Project and explore its many compelling interviews: https://www.hbs.edu/creating-e....merging-markets/Page

This video demonstrates Laparoscopic Cholecystectomy Fully Explained Skin-to-Skin Video with Near Infrared Cholangiography performed by Dr R K Mishra at World Laparoscopy Hospital. A laparoscopic cholecystectomy is a minimally invasive surgical procedure that involves removing the gallbladder. It is typically performed using small incisions in the abdomen, through which a laparoscope (a thin tube with a camera and light) and surgical instruments are inserted. The surgeon uses the laparoscope to visualize the inside of the abdomen and to guide the instruments in removing the gallbladder.
Near-infrared cholangiography is a technique that uses a special camera and fluorescent dye to visualize the bile ducts during surgery. The dye is injected into the cystic duct (the tube that connects the gallbladder to the bile ducts) and the camera detects the fluorescence emitted by the dye, allowing the surgeon to see the bile ducts more clearly.
The combination of laparoscopic cholecystectomy and near-infrared cholangiography has become a standard of care in many hospitals and surgical centers. It allows for a more precise and efficient surgery, reducing the risk of complications such as bile duct injury.
The use of indocyanine green (ICG) with near-infrared imaging during laparoscopic cholecystectomy has several advantages. Here are some of them:
Better visualization of the biliary anatomy: ICG with near-infrared imaging allows for better visualization of the biliary anatomy during surgery. This helps the surgeon identify important structures, such as the cystic duct and the common bile duct, and avoid injuring them.
Reduced risk of bile duct injury: With better visualization of the biliary anatomy, the risk of bile duct injury during surgery is reduced. Bile duct injury is a serious complication that can occur during laparoscopic cholecystectomy and can lead to long-term health problems.
Improved surgical precision: ICG with near-infrared imaging also improves surgical precision. The surgeon can better see the tissues and structures being operated on, which can help reduce the risk of bleeding and other complications.
Shorter operating time: The use of ICG with near-infrared imaging can shorten the operating time for laparoscopic cholecystectomy. This is because the surgeon can more quickly and accurately identify the biliary anatomy, which can help streamline the surgery.
Overall, the use of ICG with near-infrared imaging is a valuable tool in laparoscopic cholecystectomy that can improve surgical outcomes and reduce the risk of complications.
Like any surgical procedure, laparoscopic cholecystectomy (gallbladder removal) has potential complications. Here are some of the most common ones:
Bleeding: Bleeding during or after the surgery is a possible complication of laparoscopic cholecystectomy. Most cases are minor and can be easily controlled, but in rare cases, significant bleeding may require a blood transfusion or even additional surgery.
Infection: Any surgical procedure carries a risk of infection. After laparoscopic cholecystectomy, there is a risk of infection at the site of the incisions or within the abdomen. Symptoms may include fever, pain, redness, or drainage from the incision sites.
Bile leakage: In some cases, a small amount of bile may leak from the bile ducts into the abdominal cavity after gallbladder removal. This can cause abdominal pain, fever, and sometimes requires further surgery or treatment.
Injury to nearby organs: During the surgery, there is a small risk of unintentional injury to nearby organs such as the liver, intestines, or bile ducts. This can cause additional complications and may require further treatment.
Adverse reactions to anesthesia: As with any surgery requiring general anesthesia, there is a small risk of adverse reactions to the anesthesia, such as an allergic reaction, respiratory problems, or heart complications.
Most patients recover without complications following a laparoscopic cholecystectomy, but it is important to discuss any concerns or questions with your surgeon beforehand.
Contact us
World Laparoscopy Hospital
Cyber City, Gurugram, NCR Delhi
INDIA : +919811416838
World Laparoscopy Training Institute
Bld.No: 27, DHCC, Dubai
UAE : +971525857874
World Laparoscopy Training Institute
8320 Inv Dr, Tallahassee, Florida
USA : +1 321 250 7653
Regenerate response

At Nationwide Children’s, our Department of General Pediatric Surgery provides comprehensive surgical care for infants, children and adolescents with congenital and acquired conditions, including major congenital anomalies, traumatic and thermal injuries, and tumors. As the second largest pediatric treatment center in the United States our surgeons perform more than 4,000 operative procedures every year. We are dedicated to clinical excellence, generation of new knowledge through research and the training of the next generation of leaders in children’s surgery. Under the umbrella of a unified program, 11 surgical departments share a common mission, philosophy and approach to patient care.
Pediatric Surgery Program: https://bit.ly/3t4QZef
Pediatric Surgery Fellowship and Residency: https://bit.ly/3qWAWwd
Meet our Pediatric Surgery Team: https://bit.ly/3n39dJh
Fellowship Programs: https://bit.ly/3EX1JNX
Surgical Services: https://bit.ly/3eYDlB8

General Examination - Clinical Skills OSCE - Dr Gill
The general examination is one of those early exams, which is essentially used to start medical students off with their clinical skills studies.
In the real world, it's mainly used with regard to gaining an overview of a patient, such as for a medical check up, or a baseline examination, for example, a health report.
They have been a couple of comments about the pulse monitor used in the video. For those who are interested. I’ve reached out to the manufacturer, and they’ve requested that the following code is provided to viewers, in order to get 20% off, if they decide on themselves.
Product model number: Vibeat SP20
Official Website: https://vibeatstore.com/produc....ts/sp20-handheld-pul
Special 20% OFF code: JAMES
--------------
Different medical schools, nursing colleges and other health professional courses will have their own preferred approach to a clinical assessment - you should concentrate on THEIR marks schemes for your assessments.
Some people watching this video may experience an ASMR effect
#DrGill #Asmr #Clinicalskills
#drgill #clinicalskills #asmr

Having surgery can be frightening for anyone, but it's especially scary for kids who don't always understand what's going on, or what the grown-ups are saying. We're here to help!
Join Avrie, who had surgery at the Sacred Heart Children's Hospital pediatric surgery center in Spokane, WA. Maybe after watching and hearing her story, you and your kiddo will feel better about having surgery in the hospital.
Follow Avrie's trip - from check-in, vital signs and pre-op checks; meeting the doctor who will do his surgery, along with the anesthesiologist, surgery nurse and the Child Life Specialist; the trip to the Operating Room; waking up in the recovery room with his mom by his side; and getting ready to go home.
To learn more about the pediatric surgery center at Sacred Heart Children's Hospital, visit https://washington.providence.....org/locations-direct

Most people develop several moles (nevi) throughout adulthood. Moles can be found anywhere on the body, usually in sun-exposed areas, and are usually brown, smooth, and slightly raised. In most cases, a nevus is benign and doesn't require treatment. Rarely, they turn into melanoma or other skin cancers. A nevus that changes shape, grows bigger, or darkens should be evaluated for removal.
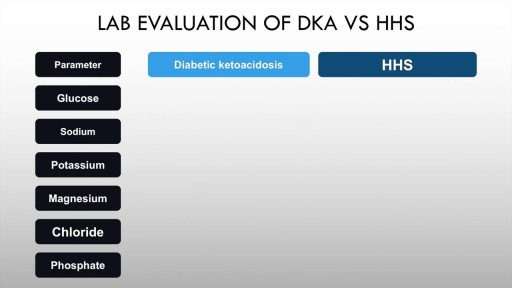
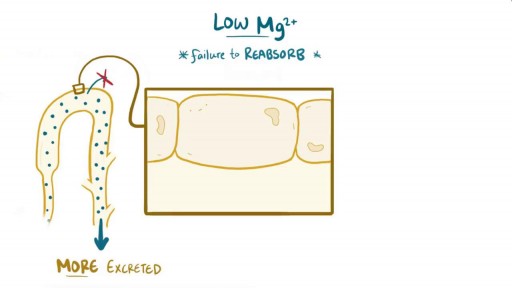
Diabetic ketoacidosis is an acute complication of uncontrolled hyperglycaemia characterised by high anion gap metabolic acidosis, dehydration and other metabolic abnormalities. Upto half of patients with Type 1 diabetes mellitus may have DKA. The incidence in T2DM is also rising. Precipitants include acute illness such as myocardial infarction, trauma and infection. Paitents of diabetic ketoacidosis may present with vomiting, pain abdomen and lethargy. Mental obtundation may also be present. Management of diabetic ketoacidosis revolves around administration of IV normal saline, insulin, replacement of potassium with frequent monitoring of sugars and electrolytes.