Top videos
Urogenital neoplasms spreading to the inguinal lymph nodes are penile carcinoma (the most frequent), urethral and scrotum cancers, tumors of the testis with scrotal violation. Penile carcinoma is an uncommon malignant disease and accounts for as many 0.4-0.6% of male cancers. Most patients are elder...ly. It rarely occurs in men under age 60 and its incidence increases progressively until it reaches a peak in the eighth decade 1. The risk of a lymph node invasion is greater with high grade and high stage tumors 2. Some investigators have reported the inaccuracy of the sentinel node biopsy 3, 4, described by Cabanas 5. Patients with metastatic lymph node penis cancer have a very poor prognosis if penectomy only is performed. Ilioinguinal lymphadenectomy is basically carried out as a treatment modality and not only as a staging act. Patients with lymph node invasion have a 30-40% cure rate. Ilioinguinal lymphadenectomy should be also performed in patients with disseminated neoplasms for the local control of the disease. The 5 years survival rate of patients with clinically negative lymph nodes treated with a modified inguinal lymphadenectomy is 88% versus 38% in patients not initially treated with lymphadenectomy 6. This video-tape clearly shows a therapeutic algorithm, the anatomy of the inguinal lymph nodes, according to Rouviere 7 and Daseler 8, the radical ilioinguinal node dissection with transposition of the sartorius muscle and the modified inguinal lymphadenectomy proposed by Catalona 9. References: 1. Lynch D.F. and Schellhammer P: Tumors of the penis. In Campbell’s Urology Seventh Edition, edited by Walsh P.C., Retik A.B., Darracott Vaughan E. and Wein A.J. W.B. Saunders Company, Vol. 3, chapt. 79, p. 2458, 1998. 2. Pizzocaro G., Piva L., Bandieramonte G., Tana S. Up-to-date management of carcinoma of the penis. Eur. Urol. 32: 5-15, 1997 3. Perinetti E., Crane D.B. and Catalona W.J. Unreliability of sentinel lymph node biopsy for staging penile carcinoma. J. Urol. 124: 734, 1980 4. Fowler J.E. Jr. Sentinel lymph node biopsy for staging penile cancer. Urology 23: 352, 1984 5. Cabanas R.M. An approach for the treatment of penile carcinoma. Cancer 39: 456, 1977 6. Russo P. and Gaudin P. Management strategies for carcinoma of the penis. Contemporary Urology;5:48-66, 2000 7. Rouviere H. Anatomy of the human lymphatic system. Edwards Brothers, p. 218, 1938 8. Daseler E.H., Anson B.J., Reimann A.F. Radical excision of the inguinal and iliac lymph glands: a study based on 450 anatomical dissections and upon supportive clinical observations. Surg. Gynecol. Obstet. 87: 679, 1948 9. Catalona W.J. Modified inguinal lymphadenectomy for carcinoma of the penis with preservation of saphenous veins: technique and preliminary results. J. Urol. 140: 306-310, 1988

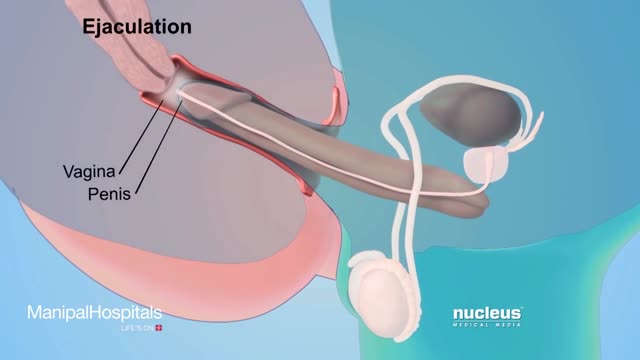
Your baby's sex is set at conception. At around 7 weeks, your baby's internal sex organs – such as ovaries and testes – begin to form in the abdomen. Male and female sex organs and genitalia look the same at this stage because they're derived from the same structures. At around 9 weeks, boys and girls begin to develop differently. In girls, a tiny bud emerges between the tissue of the legs. This bud will become the clitoris. The membrane that forms a groove below the bud separates to become the labia minora and the vaginal opening. By 22 weeks, the ovaries are completely formed and move from the abdomen to the pelvis. They already contain a lifetime supply of 6 million eggs. In boys, the bud develops into the penis and starts to elongate at around 12 weeks. The outer membrane grows into the scrotal sac that will later house the testicles. By 22 weeks, the testes have formed in the abdomen. They already contain immature sperm. Soon they'll begin their descent to the scrotum, but it's a long journey. They'll reach their destination late in pregnancy, or for some boys, after birth. If you're eager to find out whether you're having a girl or a boy, you'll have to wait until you're at least 17 weeks pregnant. That's when the genitals have developed enough to be seen on an ultrasound.
Fertilization of the egg with sperm generally occurs during the two weeks following the first day of your last menstrual period.1 The week of pregnancy that you are entering is dated from the first day of your last period. This means that in the first two weeks or so, you are not actually pregnant - your body will be preparing for ovulation as normal.

The pelvic floor or pelvic diaphragm is composed of muscle fibers of the levator ani, the coccygeus, and associated connective tissue which span the area underneath the pelvis. The pelvic diaphragm is a muscular partition formed by the levatores ani and coccygei, with which may be included the parietal pelvic fascia on their upper and lower aspects. The pelvic floor separates the pelvic cavity above from the perineal region (including perineum) below.
The right and left levator ani lie almost horizontally in the floor of the pelvis, separated by a narrow gap that transmits the urethra, vagina, and anal canal. The levator ani is usually considered in three parts: pubococcygeus, puborectalis, and iliococcygeus. The pubococcygeus, the main part of the levator, runs backward from the body of the pubis toward the coccyx and may be damaged during parturition. Some fibers are inserted into the prostate, urethra, and vagina. The right and left puborectalis unite behind the anorectal junction to form a muscular sling . Some regard them as a part of the sphincter ani externus. The iliococcygeus, the most posterior part of the levator ani, is often poorly developed.
The coccygeus, situated behind the levator ani and frequently tendinous as much as muscular, extends from the ischial spine to the lateral margin of the sacrum and coccyx.
The pelvic cavity of the true pelvis has the pelvic floor as its inferior border (and the pelvic brim as its superior border.) The perineum has the pelvic floor as its superior border.
Some sources do not consider “pelvic floor” and “pelvic diaphragm” to be identical, with the “diaphragm” consisting of only the levator ani and coccygeus, while the “floor” also includes the perineal membrane and deep perineal pouch. However, other sources include the fascia as part of the diaphragm. In practice, the two terms are often used interchangeably.
Inferiorly, the pelvic floor extends into the anal triangle.